DOG BLOG
Musings
Use of CBD to Treat Canine Seizures
I am glad to see that CBD, oftentimes hailed as a 'miracle drug,' is getting the much-deserved attention it merits. As many who know me or have read my articles are aware that I have been using CBD on my Wolfhounds for more than a decade to treat seizures in two bitches that we determined were caused by Neospora Caninum with latent, chronic infections resulting in multifocal brain lesions and or inflammation of the CNS (Central Nervous System) Granulomatous meningoencephalomyelitis (GME). Technically, without an MRI or a post-mortem to confirm, we would still be obligated to classify these as idiopathic in nature.
The AKC Canine Health Foundation published a study in March 2024 titled "Evidence for the Use of CBD to Treat Canine Idiopathic Epilepsy."
I am glad to see that CBD, oftentimes hailed as a 'miracle drug,' is getting the much-deserved attention it merits. As many who know me or have read my articles are aware that I have been using CBD on my Wolfhounds for more than a decade to treat seizures in two bitches that we determined were caused by Neospora Caninum with latent, chronic infections resulting in multifocal brain lesions and or inflammation of the CNS (Central Nervous System) Granulomatous meningoencephalomyelitis (GME). Technically, without an MRI or a post-mortem to confirm, we would still be obligated to classify these as idiopathic in nature.
I won't delve into the details of Neospora here, as I've already published several posts and articles on my website that thoroughly discuss the serious nature of this parasitic disease. You can click here to learn more about Canine Neospora and the subsequent Update on Neospora. However, it's important to note that this disease is more concerning than Lyme Disease, particularly as it cannot be eradicated from the body. This is especially true if the Indirect Fluorescent Antibody Test (IFA) shows a high titer level in the blood (for instance, 1:200 or 1:800), indicating an active infection. Typically, a titer of 1:50 or above is considered positive for prior exposure.
Antibiotics (such as Clindamycin) can effectively treat the disease. Still, I am convinced that it can go dormant and reactivate later. The same is true for Lyme disease, and I stand firm in this belief. Again, I regard Neospora to be far more serious. Having experienced its symptoms firsthand, I never want to face this disease in my hounds again, as I believe it is a terminal condition.
Let's return to the topic of CBD. My experience with CBD and seizures, though limited to two female hounds, spans well over a decade. Still, I can confidentially state that the CDB had miraculous effects in treating and minimizing their seizures. Cinneide lived to be 11 years old, and though Kellyanne lived to be 10, she ultimately succumbed to her illness as her body could no longer withstand it. It's important to note that the dosage and quality of CBD play a crucial role.
I use R&R Medicinals' Unflavored 5,000 mg Multifunctional CBD Tincture. The necessary amount of CBD corresponds to the hound's weight and severity of the seizures; for instance, Kellyanne weighed 150 pounds, and, towards the end, she was receiving 95mg—about half a dropper—twice a day. I typically administer it around 30 minutes before meals.
If you're introducing CBD to your Irish Wolfhound to help manage seizures, it's advisable to start with a lower dosage tailored to their weight and the severity of the seizures. As a starting point, consider using one-quarter of a dropper, which is approximately 48mg, taken twice daily for about five days. After that, you can increase the dosage to half a dropper, which is about 95mg.
For a larger male Wolfhound weighing around 175 lbs with seizures, I recommend starting with at least 75mg twice daily, then gradually increasing to three-quarters of a dropper, or approximately 142mg each time. If you notice that the seizures occur less frequently and with reduced intensity, you can maintain that dosage. However, if there's no improvement, feel free to raise it to a full dropper twice daily. If you don't see any positive changes after using CBD for at least a month, it would undoubtedly come as a surprise.
In the end, both Kellyanne and Cinneide experienced a remarkable transformation in their seizure patterns. They shifted from having Grand Mal seizures almost daily, often in clusters, to seeing them occur only once every two to three months. Additionally, the severity and intensity of their seizures were significantly reduced; they no longer experienced Grand Mal episodes.
From my experience, I firmly believe that CBD is a life-saving remedy for dogs with seizures. It has the potential to significantly improve the quality of life for our beloved pets, offering hope and comfort to dog owners facing this very challenging and demanding condition.
Mammary Tumors
I make it a point to regularly check the undersides of my older female wolfhounds’ abdomens and teats for any signs of mammary tumors. In my lineage, I've noticed a pattern with certain bitches appearing more prone to developing these tumors. Detected early, I have them surgically removed and biopsied, usually revealing benign or mixed cell types. I ensure these tumors are taken out, and thanks to this proactive approach, my bitches typically live to around 10 years without any cancer issues.
I make it a point to regularly check the undersides of my older female wolfhounds’ abdomens and teats for any signs of mammary tumors. In my lineage, I've noticed a pattern with certain bitches appearing more prone to developing these tumors. Detected early, I have them surgically removed and biopsied, usually revealing benign or mixed cell types. I ensure these tumors are taken out, and thanks to this proactive approach, my bitches typically live to around 10 years without any cancer issues.
Make it a routine to check your females every month to catch any nodules early! If you notice a nodule that feels hard between your fingers, even if it's smaller than a marble, it's important to schedule an appointment with the Veterinarian. They will examine it, confirm its presence, and may schedule your female hound for minor surgery if needed. However, I usually do not sit and wait to see if it gets larger. I have it removed.
Ballyhara Kellyanne
On this surgery topic, it's crucial to first check out my insights on anesthesia for Wolfhounds. Many veterinarians who aren't familiar with Sighthounds mistakenly believe there’s no difference in how to sedate or anesthetize them compared to typical breeds. However, that couldn't be further from the truth. With Sighthounds, the saying, “I have a feeling we’re not in Kansas anymore,” is so applicable. It means that the veterinarian must step out of their usual comfort zone and into a different realm of diagnostics and care altogether.
As a devoted owner, you must stand up for your Wolfhound, as they are unable to advocate for themselves. Being informed is essential. You must familiarize yourself with specific medications and understand their sensitivities to sedation and anesthesia. This knowledge is crucial. Read more about all of this on my anesthesia webpage here on Ballyharairishwolfhounds.com.
For example, in any major surgery on a Wolfhound, unless you have tested for and have knowledge that your Wolfhound does not carry the Delayed Post-Operative (DEPOH) gene then the Veterinarian should administer either Aminocaproic Acid (Amicar®) or Tranexamic Acid, (Lysteda®) one hour before surgery via IV and then the Owner administers it orally every 8 hours afterward for five days. Many veterinarians are unaware of this issue and mistakenly believe that a pre-surgical coagulation panel, consisting of a combination of PT, PTT, and possibly von Willebrand factor testing, is sufficient. Again, they would be very wrong — instead, this could be a life-threatening mistake.
Many veterinarians typically administer Torbugesic as a pre-anesthetic to ease the anesthesia process. However, I do not permit this for my Wolfhounds due to their adverse reactions to opioid medications. They often experience respiratory depression, and one of my females even had a severe anaphylactic reaction that raised concerns about her tongue swelling and potentially choking her. As a result, all my Wolfhound records at the veterinary clinic are clearly marked with a "DO NOT ADMINISTER OPIODS" directive.
We administer propofol to induce sedation directly, and the hound is monitored constantly with EKG, PaO2, SpO2, and blood pressure. Even though propofol is a fast-acting agent with rapid recovery for most breeds -- it can be prolonged in Sighthounds. Mine can take a minimum of 30 minutes, even after minimal propofol induction, for a simple surgery such as removing a nodule. I also decline the typical pain relievers during the surgery and for the hound afterward.
Instead, depending on the surgical procedure (not to include a C-section), I have used Tramadol and Gabapentin in the past with good success, as well as Deramaxx as a pain reliever. An interesting side note about Tramadol is that if your hound has Kennel Cough, also known as Adenovirus type 2 (CAV-2), then Tramadol is prescribed to relieve the coughing.
Years ago, I had one or more hounds who tolerated Meloxicam, a nonsteroidal anti-inflammatory drug, without any issues. However, everything changed with Ballyhara Kellyanne, who produced two litters for me. She had a shocking and severe reaction to Meloxicam. Since then, I’ve stopped using it in my bloodlines entirely, as her response panicked us, and her offspring could have inherited the same sensitivity. Similarly, I avoid using Rimadyl or Carprofen; I am aware that, in certain breeds, their side effects can include seizures, vomiting, black tarry stools, and jaundice.
If you notice a nodule on your hound, don’t hesitate to address it right away. It’s common for female dogs to develop several nodules on their mammary glands, so don’t be too alarmed if you find more than one. For the latest information on mammary tumors, be sure to check out the resources available from the AKC Canine Health Foundation, New Treatment Strategies for Canine Mammary Tumors.
Canine Heart Health and Genetic Testing
Canine genetic tests are important and must be interpreted together. Phenotype refers to a dog’s observable traits, whereas genotype refers to a dog’s genetic constitution. Phenotypic tests are typically performed by a veterinarian or board-certified cardiologist. DNA tests can be used to determine a dog’s genotype for specific genetic variants, but phenotype tests are required to obtain a diagnosis of heart disease.
The following article published by the AKC is the newest article on Heart Health and is essential for many purposes. Many companion owners need to be aware of the warnings and advice of a breed's Parent Club; in this case, it would be the Irish Wolfhound Club of America (IWCA.)
Unfortunately, the IWCA is noticeably absent from this article in providing valuable and critical guidance to Wolfhound owners, as cardiac disease is one of the leading causes of death in Wolfhounds. In my opinion, based on the number of emails and requests I receive, it is the leading cause of death as, sadly, countless breeders do not educate their IW owners about Atrial Fibrillation and Dilated Cardiomyopathy (DCM), as well, Ventricular Premature Complexes (VPC). Many wolfhounds die needless early deaths because they were not properly and annually tested.
My policy has always been to inform Wolfhound owners that heart testing is imperative and mandatory beginning at age two and annually after that. Any advanced cardiac testing MUST include Auscultation, EKG and Echocardiograms.
The IWCA website states: It is important to remember that testing is important for all Irish Wolfhounds, not just those who are used for breeding. Early detection of changes in health often leads to a better quality of life for your dog. All Irish Wolfhounds may benefit when your dog participates in a health study that increases our knowledge…Cardiac screening in IWs should always be performed by a Board-certified veterinary cardiologist.
Canine Heart Health and Genetic Testing
By Claire Wiley, VMD, DACVIM
Published: Feb 22, 2024
Canine genetic tests are important and must be interpreted together. Phenotype refers to a dog’s observable traits, whereas genotype refers to a dog’s genetic constitution. Phenotypic tests are typically performed by a veterinarian or board-certified cardiologist. DNA tests can be used to determine a dog’s genotype for specific genetic variants, but phenotype tests are required to obtain a diagnosis of heart disease.
The heart is a complex organ that can manifest disease in multiple ways. Some heart diseases are present at birth (congenital), whereas others develop as the dog ages. These conditions can lead to symptoms such as coughing, lethargy, exercise intolerance, fainting, and even sudden death if left untreated. Some common heart diseases seen in dogs include:
1. Degenerative Mitral Valve Disease (DMVD)
This middle to old age disease is the most common of all canine heart diseases. One of the heart valves, the mitral valve, becomes thickened and damaged as the dog ages. The valve can leak blood and cause heart enlargement that can progress to congestive heart failure (CHF). Although small breed dogs are more prone to developing this disease, any dog can be affected. At the time of writing this article, no genetic tests are available to help predict the occurrence of this disease.
2. Dilated Cardiomyopathy (DCM)
With DCM, the second most common form of heart disease in dogs, the heart chambers become enlarged (dilated) and the walls become thin. DCM can have multiple causes, including inherited and nutritional. Multiple genetic variants have been identified that are associated with DCM that are typically breed-specific tests. Although some of these variants are inherited in a simple Mendelian fashion, others are complex and represent risk factors. Age of onset can vary from breed to breed. For example, Portuguese Water Dogs can develop an inherited, juvenile form that typically manifests before 6 months of age, called Juvenile Dilated Cardiomyopathy.
Phenotypic tests are crucial for evaluating the current function of the heart. Some common tests include:
1. Auscultation: Auscultation involves listening to the heart sounds using a stethoscope. Abnormalities such as murmurs, irregular rhythms, or gallops can indicate underlying cardiac issues.
2. Echocardiography: Echocardiography, or cardiac ultrasound, provides detailed images of the heart’s structure and function. It helps assess chamber sizes, valve function, and overall cardiac performance.
3. Electrocardiography (ECG or EKG): ECG records the electrical activity of the heart, helping identify arrhythmias and conduction abnormalities.
4. Chest radiographs: Radiographs offer valuable insights into the size and shape of the heart, as well as detecting signs of congestive heart failure, such as pulmonary edema or pleural effusion.
5. Holter Monitoring: Holter monitoring involves continuous ECG recording over 24-48 hours, allowing for the detection of intermittent arrhythmias.
The American Boxer Club, Inc., for example, recommends routine Holter monitoring annually for breeding to help decrease the incidence of Boxer Cardiomyopathy.
Genetic testing related to canine cardiac health is most important for informing breeding practices when selecting breeding pairs. The AKC DNA Program is about to launch genetic testing in the coming months, and several genetic variants for heart health are included in this panel.
Parent Club Recommended DNA Cardiac Health Tests:
Dilated Cardiomyopathy (Schnauzer Type) This specific genetic variant investigates a deletion in the RBM20 gene.
Juvenile Dilated Cardiomyopathy in Portuguese Water Dogs (Available only through PennGen) This genetic variant investigates a locus on canine chromosome 8.
Other AKC DNA + Health Heart Tests:
Cardiomyopathy and Juvenile Mortality. This genetic variant is associated with severe heart disease that can cause death from heart failure by 8 weeks of age.
Dilated Cardiomyopathy (Doberman Pinscher Type Risk Factor, Variant 1)
This specific genetic variant investigates a deletion in the PDK4 gene and is associated with disease in Doberman Pinschers, and its association with DCM in other breeds is not clear. This genetic variant is inherited in an autosomal dominant manner with incomplete penetrance. In other words, not every dog with this genetic variant goes on to develop the disease DCM.
Dilated Cardiomyopathy (Doberman Pinscher Type Risk Factor, Variant 2)
This specific genetic variant investigates a single nucleotide polymorphism (SNP) in the TTN gene and is associated with disease in Doberman Pinschers.
Canine genetic testing for heart disease represents a valuable tool in the arsenal against decreasing the risk of producing cardiac conditions in dogs. By leveraging the power of genetics, veterinarians and dog owners can work together to identify at-risk individuals, implement preventive measures, and provide personalized care to improve the overall cardiac health and well-being of our beloved canine companions. Each known genetic variant for DCM will be discussed in more detail in the coming months. As research continues to advance, genetic testing holds the promise of further enhancing our understanding and management of canine heart disease.
Citations:
1. Werner P, Raducha MG, Prociuk U, Sleeper MM, Van Winkle TJ, Henthorn PS. A novel
locus for dilated cardiomyopathy maps to canine chromosome 8. Genomics. 2008
Jun;91(6):517-21.
1. Harmon MW, Leach SB, Lamb KE. Dilated Cardiomyopathy in Standard Schnauzers:
Retrospective Study of 15 Cases. J Am Anim Hosp Assoc. 2017 Jan/Feb;53(1):38-44.
3. Gurtner C, Hug P, Kleiter M, Köhler K, Dietschi E, Jagannathan V, Leeb
T. YARS2 Missense Variant in Belgian Shepherd Dogs with Cardiomyopathy and
Juvenile Mortality. Genes (Basel). 2020 Mar 14;11(3):313. PubMed: 32183361
4. Meurs KM, Lahmers S, Keene BW, White SN, Oyama MA, Mauceli E, Lindblad-Toh K. A
splice site mutation in a gene encoding for PDK4, a mitochondrial protein, is associated
with the development of dilated cardiomyopathy in the Doberman pinscher. Hum
Genet. 2012 Aug; 131(8):1319-25.
5. Owczarek-Lipska M, Mausberg TB, Stephenson H, Dukes-McEwan J, Wess G, Leeb T. A
16-bp deletion in the canine PDK4 gene is not associated with dilated cardiomyopathy
in a European cohort of Doberman Pinschers. Anim Genet. 2013 Apr;44(2):239.
6. Meurs KM, Friedenberg SG, Kolb J, Saripalli C, Tonino P, Woodruff K, Olby NJ, Keene
BW, Adin DB, Yost OL, DeFrancesco TC, Lahmers S, Tou S, Shelton GD, Granzier HG. A
missense variant in the titin gene in Doberman pinscher dogs with familial dilated
cardiomyopathy and sudden cardiac death. Hum Genet. 2019 May;138(5):515-524.
Discoveries: Advances in Canine Bone Cancer Research
New treatments are needed for canine bone cancer. Current treatment options include surgical removal of the tumor and chemotherapy to treat metastatic disease (cancer spread to distant parts of the body). Unfortunately, surgery can have complications, not all dogs are good candidates for surgery due to other health problems, and many affected dogs develop metastatic disease and only survive for one year or less after diagnosis.
AKC Canine Health Foundation Discoveries
By Sharon Albright, DVM, CCRT
Manager of Communications & Veterinary Outreach, AKC Canine Health Foundation
New treatments are needed for canine bone cancer. Current treatment options include surgical removal of the tumor and chemotherapy to treat metastatic disease (cancer spread to distant parts of the body). Unfortunately, surgery can have complications, not all dogs are good candidates for surgery due to other health problems, and many affected dogs develop metastatic disease and only survive for one year or less after diagnosis.
Since 1995, the AKC Canine Health Foundation (CHF) and its donors have invested more than $3 million in 42 studies to improve outcomes for dogs with bone cancer. Since canine bone cancer is similar to human adolescent bone cancer, what we learn about dogs could also help children affected by this devastating disease. There is exciting progress toward that goal.
A recent study conducted by 2016 CHF Clinician-Scientist Fellow Dr. Shirley Chu found that genetic mutations in canine bone cancer cells were similar even in different locations within a patient. However, the mutations were unique to each individual dog studied. Additional research could explore if these mutation differences indicate subtypes of bone cancer that should be studied to offer more targeted and effective treatments and a more accurate prognosis for affected dogs.
Cudama Santa at Ballyhara
Another study showed that a unique form of bone cancer that strikes Irish Wolfhounds at a young age (less than 5 years old) is highly heritable with 65% of disease development attributed to genetic factors. Future studies will explore the specific genetic mutations that contribute to this form of cancer.
Investigators at Tufts University described the DNA of canine bone cancer cell cultures, confirming that these cultured cells adequately represent natural disease. This means that scientists can study these cell cultures to see which chemical pathways are disrupted by cancerous mutations and could be targeted by new treatments.
Finally, an exciting line of study at the Virginia-Maryland College of Veterinary Medicine is concentrating on a treatment protocol for canine bone cancer using the technology known as histotripsy. This focused ultrasound treatment mechanically disintegrates tumor tissue without affecting surrounding muscle or nerve cells. The treatment was first tested on bone cancer tissue samples removed from donor dogs. After this successful study, histotripsy was used to treat five client-owned dogs with suspected bone cancer. These clinical trial participants received standard limb amputation surgery 1-2 days after the histotripsy treatment. They showed no significant adverse effects from the treatment and microscopic examination showed that histotripsy effectively disintegrated the tumor tissue while sparing surrounding normal tissues.
Exploration of histotripsy as a new treatment for bone cancer continues, as CHF funding is helping scientists determine the best way to monitor response to treatment and how it impacts the immune system. Other newly awarded grants
will examine interactions between bone cancer and immune system cells – exploring how immune cells gain access to important regions within bone tumors and if and how they are manipulated to help the tumor grow. Study also continues on the genetic mutations found in bone cancer cells and how we can use them to develop better tests and treatments. And the exciting prospect of a blood test for early detection of canine bone cancer is under development at the University of Minnesota.
Canine bone cancer is a devastating diagnosis for dogs and their families. But thanks to the dedication of CHF’s donors and funded investigators, there is hope. Hope for better diagnostic tests. Hope for more successful and less invasive treatment options. And hope for longer, healthier lives for the dogs we love. Learn more about CHF-funded bone cancer research, including how you can help, at akcchf.org/osteosarcomaRPA.
Best to Grind Your Dogs Heartworm Pill!
Grind your dog’s and cat’s heartworm preventatives! If your pet does not chew the pill then it loses its effectiveness!
Just because we're entering into the Autumn season does not mean that dog owners can slack off about giving heartworm preventative. On my website, under Recommended Vaccinations & Wormers, I have advice from Dr. Jean Dodds, Hemopet.
She advises using heartworm preventatives for healthy dogs if the ambient temperature is above 57 degrees Fahrenheit (14 degrees Centigrade) for approximately two weeks and mosquitoes are prevalent. A basic rule of thumb is Mid-April through November for the majority of the country and basically year-round for the southern states.
However, we are experiencing climate change worldwide. Therefore, it would be wise for those living in the four-seasons regions to keep dosing with heartworm preventative through December just to be safe. This past late Autumn into early winter, I recall mowing my pastures despite the calendar being the end of December! At the same time, be prepared to begin dosing earlier than April if there is a much warmer than usual forecast. Still, first, you must have a heartworm blood test performed. I prefer Snap 4DX tests, which also screen for Anaplasma, Ehrlichia, and Lyme tick diseases.
The most important tip for everyone to know when dispensing heartworm preventatives is that the dog MUST chew the tablet. Since many heartworm preventatives are in chewables forms, people get complacent and think that when they give it to their dog, they'll munch on it. But, if your dogs are like mine, they simply swallow it without chewing. So my policy is to GRIND the pills into tiny pieces or even a powder in a small bowl and add it to a small handful of ground meat. Then I administer it to each of the hounds. This method guarantees that the pill has been crushed without chewing!
Why the big deal? Because pharmaceutical companies require dogs to chew and NOT to swallow their preventative whole for the effectiveness of the pill. Many, many dog owners are completely unaware of this issue. Over the years, I have heard stories about dogs diagnosed with the disease despite taking monthly preventatives. The owners contacted the company and were informed that, most likely, their dog never chewed the pill! That is not what you want to hear after the fact.
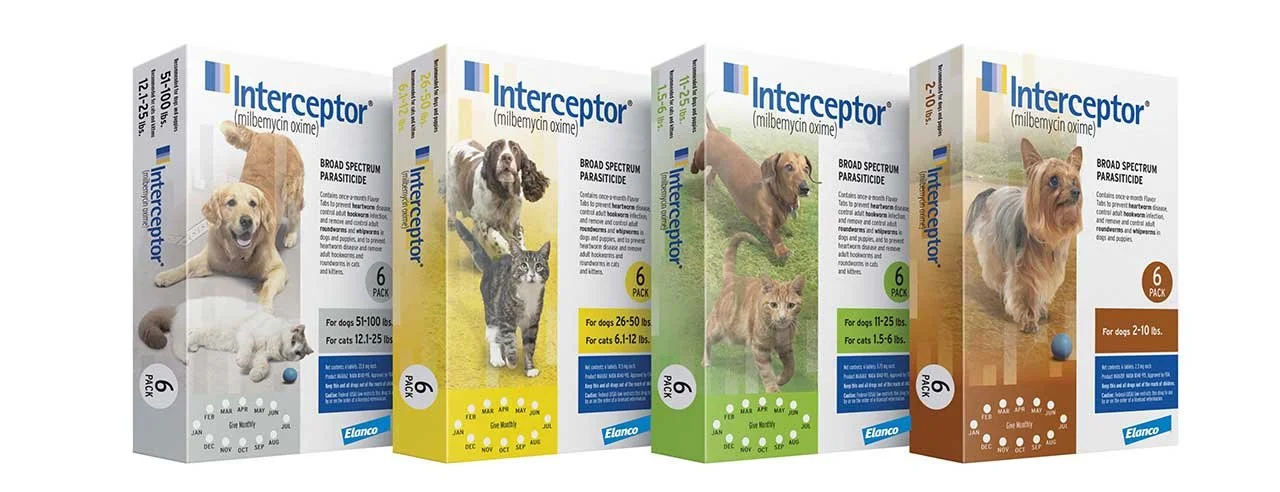
Lastly, I urge you to use heartworm preventative medicines. But choose carefully, as there are several options on the market with varying degrees of side effects for specific breeds. For example, some Herding Breed dogs have a genetic mutation that makes them dangerously oversensitive to ivermectin, as well as white colored-dogs, and dogs prone to seizures. Additionally, Sighthounds are very sensitive and are best suited with plain milbemycin oxime. I discuss heartworm preventatives and wormers in detail on my website, so please take a moment and visit Recommended Vaccinations & Wormers.
Post-Estrus Depression Update
More updates on my "Canine Post-Estrus Depression" DogBlogMusings article, as my website analytics inform me that this topic is the second most popular page on my entire website! This is unusual as my website welcomes a fair number of visitors regularly. I also receive email pleas for assistance on the topic. Still, the elevation in popularity on my popular website concerns me. It seems that this behavioral change in dogs is increasing considerably. Buy why?
Another update to my "Canine Post-Estrus Depression" DogBlogMusings article, as my website analytics inform me that this topic is the second most popular page on my entire website! This is unusual as my website welcomes a fair number of visitors regularly. I also receive email pleas for assistance on the topic. Still, the elevation in popularity on my popular website concerns me. It seems that this behavioral change in dogs is increasing considerably. Buy why?
I originally penned my first article (see below) with what I believed was a possible solution in the hopes that others may find it helpful. Unluckily, it was based on my experience with my fairly exclusive bloodlines meaning that this behavior was typical for my female lineages. I had not heard that other bloodlines were experiencing the same. So, of course, I offered my solution with the full knowledge that it may not work for all dogs, but even if it helped a few, it was worthwhile.
Back to why this issue is happening with such frequency now; the answer is, I don't know. Any surmising based on commonality cannot provide an explanation. Could it be commercial dog food with its common preservatives or additives? Not possible as my hounds are "Naturally Reared" and have been so for about 29 of my 39 years. Please visit my Nutrition page for those unfamiliar with this term, but the short answer is I do not feed commercial dog food.
All I can do is provide other possible solutions that I have also used to counteract the depression and lack of appetite. But first, I want to caution everyone who is searching for an answer to have your dog tested for Tick diseases. No excuses are valid such as “I haven’t seen any ticks on my dogs” or, “My dog wears a tick collar”, or “We do not have ticks in our region” or “It is winter.” Tick diseases can lie in the body and dependent on what stage they are cause symptoms or not: Acute, Subclinical, or Chronic.
Please have your Veterinarian run a SNAP 4DX PLUS test run on your dog. This test will screen for seven vector borne diseases, to include not just Heartworm but very importantly Lyme, Ehrlichia, and Anaplasma diseases. Anaplasmosis symptoms include loss of appetite and in todays environment a dog can have Anaplasmosis at any time of the year. Ehrlichia symptoms also include weight loss and inappetence. Recently, I had several bitches who were eating poorly 3-4 weeks after completion of their heat cycles. My Veterinarian and I tested with SNAP4DX and all came back positive with varying levels of Anaplasmosis and Lyme disease. As a result, they all began a drug protocol regiment of doxycycline for 30 days. Several began eating normally again shortly after.
In addition to the original suggestion of Wobenzym N Systemic Enzymes from The Garden of Life,
I also suggest R&R Medicinals as an excellent manufacturer of CBD tinctures. They do make a Full Spectrum version for pets that you can use. Follow the directions on their website, and once your dog is acclimated to it, I would increase the dosage to twice daily. As they say, consistency is essential for the best results; that is when you will see changes. If you have a giant breed, I would consider dosing up to 50 mg daily after the dog has adjusted to the initial doses over a couple of weeks.
My females come into season about every 4 - 6 months. As such, one of our girls is consistently on CBD, and she is 8 years of age. It has shortened her "downtime" of not-eating. She still experiences depression, but it is curtailed to about a week or so, whereas before CBD, she would go off her food for 3 weeks at a time. Nonetheless, while she is in her "woe is me" self-inflicted fasting, I resort to other means to get nutrition into her. These recommendations suit any dog that has gone off its food, barring severe diseases.
I take raw, pure honey that I purchase directly from the local Bee Apiarists, and I refrigerate about a cupful at a time. The refrigeration nearly solidifies the raw honey so that you can scoop out one tablespoon at a time and place it in the dog's mouth with a spoon. Let the dog swallow as they lick repeatedly and then repeat again in a few minutes. For a 140-pound dog, I give about three tablespoons of honey in this manner twice daily. My big male will go off his food when the females are in season, so I do the same for him, but his dose is much larger. He weighs about 175-pounds, so he gets about 4 Tablespoons of the refrigerated honey twice daily. If you haven't figured it out yet, administering the honey in this manner resolves the issue of significant messes. Honey is very thick and sticky and will drip everywhere if you try to use it in its liquid state right out of the jar.
Another nutritious trick I use on these dogs who are not eating is fresh eggs. First, I crack a raw egg into a small 1/4 measuring cup (adjust to a smaller size for small dogs). Then, with one hand, I open the dog's mouth and slide the egg out onto the back of their tongue while quickly closing the mouth and keeping their muzzle elevated as they swallow. I have seen improvements in their attitude and behavior after having raw honey twice daily when refusing all other foodstuffs. And don't forget the egg once per day.
Original Article on Post-Depression Follows
Possible Remedy for Canine Post-Estrus Depression
It is possible that I might have found a remedy for post-estrus depression in our female Irish Wolfhounds. For a number of veteran breeders, this is a familiar syndrome that affects wolfhound bitches typically two to three weeks after concluding their heat cycles.
First, the female canine has four cycles including before and after her reproductive period. These are Anestrus, Proestrus, Estrus, and Diestrus with the latter being the stage after mating. Anestrus is the term for quiescence or dormancy between her semi-annual or annual heat cycles. As I explained on my website page "Irish Wolfhound Spay-Neuter Considerations and Concerns," my tail-female (maternal bloodlines) endure difficult episodes two to three weeks after concluding estrus (heat cycles). They stop eating, lose weight, and are depressed which has been very worrisome. I even had a bitch once regularly lose up to 15 pounds during these depressions. I am not describing pseudopregnancy or false pregnancy in which the female's exhibit mothering behavior and bodily changes such as mammary gland enlargement, lactating, nesting, depression, even abdominal swelling.
No, what I coined post-estrus depression is more worrisome because my girls have the "woe is me" and "life is not worth living anymore" attitudes. We do everything we can to entice them to eat, yet, most of the time they turned their noses up at fresh meat, homemade chicken stock, you name it. However, recently I began trying systemic enzymes on my intact young female wolfhounds.
I have been feeding systemic enzymes for some time now in which I use Garden of Life's 'Wobenzyme' for our veteran Irish Wolfhounds. I also take them myself. Enzyme therapy is considered therapeutic "promoting health in every part of the body by reducing pain and inflammation, speeding healing, supporting a healthy immune system." You can read more about Enzymes here in this article written by Mary Straus, published in the Whole Dog Journal, July 2012 and reproduced at DogAware.com, "Proteolytic Enzymes, Enzymes for Healing Body Tissues, Not “Just” for Digestion."
I began my trial with the Wobenzyme on the two intact bitches as soon as they came into season continuing throughout and past their reproductive cycles and even today, they still receive the enzymes regularly. As usual, two weeks after the conclusion of their heat cycle the first signs of depression began and an indication of disinterest in food. However, this time I noted that both females' depression were much milder than previous post-estrus depression events. If I were to use a percentage, I would estimate that the undesirable behaviors were reduced as much as 80%. Yes, the bitches would miss a meal perhaps three times a week, but that frequency pales in comparison to previous depression events when they would go for several days without eating a thing. I have observed a marked difference in their daily behaviors and this trial has been a success. A protocol that I will continue to administer as so far it has afforded me a huge sigh of relief!
How does it work? Well, I can only hypothesize referring to the data provided in the article which states,
"Studies in the U.S. are limited, but systemic enzyme therapy has been studied and used in Germany for decades. For example, a 2008 German review of “rigorous clinical studies” published in the journal Integrative Cancer Therapies found that “systemic enzyme therapy significantly decreased tumor-induced and therapy-induced side effects and complaints such as nausea, gastrointestinal complaints, fatigue, weight loss, and restlessness and obviously stabilized the quality of life."
It is only logical that my seeing a marked improvement in their eating behavior is a possible result of what this study concluded -- systemic enzyme therapy significantly decreased nausea, gastrointestinal complaints, fatigue, and weight loss. It appears to have done so in my Irish Wolfhound bitches.
If your bloodlines, regardless of dog breed, have undergone this same depression-like event, I would encourage you to try the same.
Please know that the author cautions that Proteolytic enzymes can thin the blood and increase the risk of bleeding, especially at higher doses. Do not give to dogs with clotting disorders, gastric ulcers, or those receiving blood-thinning medications. If anemia or signs of bleeding develop, discontinue right away. High doses may cause diarrhea.
Balancing Calcium & Phosphorus For Dogs, Repost By Dr. Jean Dodds
Dr. Dodds and Hemopet advocate for the advantages of properly-balanced and prepared homemade meals for companion pets. Indeed, these include the fact that companion pet parents can control and choose ingredients, customize for age and health, and modify according to any food sensitivities and intolerances.
The following is a repost of Hemopet’s discussion on Calcium and Phosphorus ratios. The article is for the advanced student who is well informed with Natural Rearing. I would not recommend a novice simply winging it when feeding their dog a “homemade diet.” Another source that is quite good is Dr. Pitcairn’s, “Complete Guide for Natural Health for Dogs & Cats.” The link to the book is on my Diet & Nutrition page.
Balancing Calcium and Phosphorus for Dogs
February 19, 2021 / Nutrition / By Hemopet
Dr. Dodds and Hemopet advocate for the advantages of properly-balanced and prepared homemade meals for companion pets. Indeed, these include the fact that companion pet parents can control and choose ingredients, customize for age and health, and modify according to any food sensitivities and intolerances.
Yet, we understand why some veterinary professionals are concerned about homemade diets for their pet companion. And, yes, we agree with their concerns. That is why we encourage companion pet parents to work with reputable and experienced veterinary/animal nutritionists.
With that being said…what is their concern? For many, it can be the very complex mineral assessment that veterinary nutritionists need to consider for our pets, namely: The Calcium:Phosphorus Ratio.
The essential minerals of calcium and phosphorus need to be delicately and accurately balanced relative to each other. Both calcium and phosphorus are provided through foods, but an excess or a deficiency of one or the other can lead to deleterious effects on the body and health.
Vitamins D2 and its active form, D3, compound this issue of mineral balance. Their role is to enable proper absorption and uptake of calcium and phosphorus, as well as assist with other calcium and phosphorus functions in the body.
Compounding the issue even further is how the two vitamin Ds are given. Vitamin D3 (calcitriol) is not nutritionally accessible and must be added as a supplement. It is available only through sunlight, which is often insufficient these days with depletion of the ozone layer and pollution, and by supplementation. Vitamin D2 (calcidiol) needs can be achieved through dietary means.
Further, the function of vitamin D is complicated by the nature of its absorptive aid properties. Vitamin D aids the intestinal absorption of calcium, and helps ionized phosphorus (i.e. phosphate) be reabsorbed back into the bloodstream from the small intestine and kidneys.
The parathyroid gland and fibroblast growth factor 23 (FGF-23) also play important roles.
Indeed, the interactions of calcium, phosphorus and vitamin D can result in a variety of metabolic, biochemical and physiological outcomes.
Yes; it surely is confusing and complicated.
The optimal dietary calcium to phosphorus ratio in dogs should be 1.2:1 to 1.3:1. The ratio appears small, but it is significant. So, we thought we would give you two easily digestible conditions (pun intended) that illustrate the effects an imbalance of calcium and phosphorus can cause.
Calcium Excess
An easy example of excessive calcium intake is rickets-like signs in puppies or young dogs. Puppies will experience:
Bone deformation or bowed limbs
Bone pain and swelling
Fractures
Stiff gait or limp
Typically, we see rickets-like conditions with dogs fed only all-meat diets.
The remedy? Rickets-like symptoms in dogs can be reversible if caught early enough. Basically, a companion pet parent needs to balance the calcium to the phosphorus intake and add a vitamin D supplement.
Excess Phosphorus
Nutritional secondary hyperparathyroidism is an excess of phosphorus compared to calcium in the diet. When phosphate levels are maintained at untenable levels in the blood or are unmatched by sufficient calcium intake, calcium in the blood drops causing hypocalcemia. Low serum calcium, in turn, signals the parathyroid to call upon the calcium in bones to replenish what is missing in the blood. The demineralization of bones cause weakness, possible fractures and neurological dysfunction.
Again, the cause can be attributable to dogs fed only all-meat diets.
The Takeaway
Bear in mind that the two examples provided here are simple. There could be more complex and underlying conditions causing excessive or insufficient levels of calcium or phosphorus. These examples demonstrate the importance of dietary balances (particularly of minerals like calcium and phosphorus), and how easily dietary imbalances can result in health conditions.
References
Barber, Penney. “Nutritional Secondary Hyperparathyroidism.” Vetlexicon, Vetstream, www.vetstream.com/treat/canis/diseases/nutritional-secondary-hyperparathyroidism.
Brooks, Wendy. “Calcium Phosphorus Balance in Dogs and Cats .” Veterinary Partner, VIN, 5 June 2019, https://veterinarypartner.vin.com/default.aspx?pid=19239&id=4952674.
Grünberg, Walter. Disorders Associated with Calcium, Phosphorus, and Vitamin D in Dogs. Merck Veterinary Manual, Mar. 2018, https://www.merckvetmanual.com/dog-owners/bone,-joint,-and-muscle-disorders-of-dogs/disorders-associated-with-calcium,-phosphorus,-and-vitamin-d-in-dogs.
Moe, Sharon M. “Disorders involving calcium, phosphorus, and magnesium.” Primary Care vol. 35,2 (2008): 215-37, v-vi. doi:10.1016/j.pop.2008.01.007, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2486454/.
Schaefer, Carmenn, and Richard E Goldstein. “Canine primary hyperparathyroidism.” Compendium (Yardley, PA) vol. 31,8 (2009): 382-89, https://pubmed.ncbi.nlm.nih.gov/19866445/.
Shaker JL, Deftos L. Calcium and Phosphate Homeostasis. [Updated 2018 Jan 19]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279023/.
Stillion, Jenefer R, and Michelle G Ritt. “Renal secondary hyperparathyroidism in dogs.” Compendium (Yardley, PA) vol. 31,6 (2009): E8, https://pubmed.ncbi.nlm.nih.gov/19746344/.
Saving Sighthounds from Anesthetic Drug Death
Saving Sighthounds from Anesthetic Drug Death! Due to Sighthound’s peculiar quirks, they have a potentially life-threatening, slow recovery reaction to and from anesthetic drugs.
There have been a proportional number of sighthounds who have died on the operating table, especially Greyhounds, Scottish Deerhounds, and Irish Wolfhounds, and or who have had significant difficulty awakening from anesthetics….
This article is important for Sighthound owners and most certainly applies to Wolfhounds. The original article can be found here.
The locomotion of the long, lean muscles of running Greyhounds is simultaneously elegant and breathtaking. Like other ancient sighthound breeds hardwired to pursue prey by speed and sight, the Greyhound has idiosyncrasies that include having a potentially life-threatening, slow recovery from anesthetic drugs.
Identifying gene mutations responsible for breaking down, or metabolizing, commonly used drugs in Greyhounds and other sighthound breeds is the focus of research underway at Washington State University. Lead investigator Michael Court, BVSc, PhD, professor and the William R. Jones Endowed Chair, says the goal is to develop a drug sensitivity test from saliva, urine or blood that will identify dogs with a slow drug metabolism of certain drugs.
“This would allow a veterinarian to make dose adjustments or select an alternative drug for optimal drug treatment,” he says. “A personalized or individual approach to drug selection would be the ideal outcome for affected dogs.”
A veterinary anesthesiologist who has worked in research since 1983, Dr. Court is revolutionizing a cocktail drug phenotyping approach to use in dogs that will enable several drugs to be tested at the same time to determine their metabolism ratio in the body. The test would produce results classifying a dog as a slow, normal or fast metabolizer for a specific group of drugs.
“The original problem drug in sighthounds was a barbiturate, thiopental, which is used to induce anesthesia,” Dr. Court says. “Greyhound owners in Australia and the U.S. reported that it took their dogs 48 hours to stand unassisted after having thiopental anesthesia. Although thiopental is no longer used in the U.S., its use continues in most of the world. The replacement drug in the U.S. is propofol, though even with this drug, recovery in Greyhounds can be double what is normal, taking 40 minutes instead of 20 minutes.”
Since all of the problem anesthetic drugs are highly fat-soluble, the sensitivity of Greyhounds and other lean-bodied sighthounds to these drugs was originally thought to result from a reduced ability of their tissues to “soak up” the drug, keeping it away from the brain. However, more recent work has implicated a reduced ability of the dog’s liver to break down and remove the drug from the body. Specifically, there appears to be deficiency of an important drug metabolism enzyme, called cytochrome P450 (CYP).
“Using a candidate gene approach to identify gene mutations in Greyhounds that decrease anesthetic drug metabolism, we found two mutations that may explain the slow metabolism,” says Dr. Court. “One is a mutation in one of the CYP (CYP2B11) genes, and the other is in a gene for an enzyme needed for CYP to work efficiently, called P450 oxidoreductase (POR). Together, these drug-metabolizing enzymes make the drugs more water soluble, so they can be easily flushed out through the kidneys.
“Both mutations are found primarily in Greyhounds and some sighthound breeds. Rarely in non-sighthound breeds.”
Developing A Novel Drug Sensitivity Test
The sighthound adverse drug reaction research, now in phase two, focuses on developing a cocktail drug phenotyping test. Funding of $172,765 for the two-year study that began in June 2018 is provided by the AKC (American Kennel Club) Canine Health Foundation. Phase one of the research, which ran from 2016 to 2018, received funding of $150,000 from the AKC Canine Health Foundation. This work involved functional studies of the mutations in the laboratory.
“The AKC Canine Health Foundation is committed to advancing a future for personalized medicine for canine patients,” says Dr. Diane Brown, CEO of the AKC Canine Health Foundation. “We consider Dr. Court’s work in this area as an important series of first steps toward that future, and have dedicated funding to these efforts since 2016.”
Although the adverse drug reactions in sighthounds is similar to the MDR1 gene mutation in herding breeds that causes a neurotoxic reaction to ivermectin and other drugs (see below), there are differences. While the mutations in sighthounds dramatically reduce the function of the enzymes, they do not wipe them out, as occurs with dysfunction of the P-gp transporter protein in herding breeds.
“These are two different processes with the same goal, essentially trying to limit the amount of a drug that gets into the body,” Dr. Court explains. “P-gp keeps drugs out of the body, and especially the brain, by pumping the drug out. Drug-metabolizing enzymes like CYP2B11 make drugs in the body water soluble, so they can be easily flushed out, usually through the kidneys. The slow metabolism also changes the drugs chemically so they often lose their effect.”
Stephanie Martinez, PhD, a postdoctoral research associate in the Veterinary Clinical Pharmacogenetics Laboratory at Washington State University, is working with Dr. Court on the sighthound research. “In the first two-year study, we saw a significant loss of enzyme function from the mutations when we tested them in the lab,” she says.
In May 2018, Dr. Martinez adopted two retired Greyhound racers, “Seamus” and “Otis.” As a new Greyhound owner, she relates to concerns about having her dogs anesthetized for even a dental cleaning procedure. “To be honest, I am a little nervous to put them under anesthesia,” she says. “I had them genotyped right away. Both are heterozygous for one of the anesthesia adverse reaction mutations, which means they have one copy of the mutated allele, though I do not know how significantly they are affected.
“In addition to the delayed anesthesia recovery issues, some sighthound breeds like Scottish Deerhounds and Greyhounds experience bleeding issues that occur 24 to 72 hours after surgical procedures. We think it is caused by a genetic mutation that causes the blood clot to break down prematurely. Otis is homozygous for a candidate gene we’re currently investigating, which means he may experience postoperative bleeding problems.”
A separate study of delayed postoperative bleeding, funded in part by the Scottish Deerhound Club of America, is underway in conjunction with the anesthesia research. The team is seeking DNA samples from sighthounds that experienced delayed bleeding 24 to 72 hours after surgery, as well as DNA from littermates of dogs that died from this condition.
The cocktail drug phenotyping research involves testing 12 dogs with three drugs to evaluate their rate of metabolism. “The drug cocktail includes an antidepressant, which we believe will be metabolized slowly in dogs with the mutation, because it is only metabolized by CYP2B11,” Dr. Court explains. “The other drugs are an over-the-counter acid reducer and a cough suppressor. These latter two should be metabolized normally in dogs with the mutation because they are metabolized via other CYP enzymes.”
Currently, the research team is working to ensure that the three drugs can be safely given at low doses together without interfering with one another. They also want to be sure the saliva concentrations of the drugs and metabolites match the blood and urine concentrations so that saliva can be used for the test.
“The power of this approach is that we can readily test hundreds of dogs,” says Dr. Court. “Once we have this cocktail phenotyping test worked out, then we plan to use it in dogs with and without the mutations to show that the metabolism of the CYP2B11 enzyme is slow, but metabolism of the other CYP probes is normal.
“Ultimately, owners could perform a saliva test at home that would determine the ability of individual dogs to handle drugs that could be affected by rare mutations, even those not yet discovered,” he says. “The impact of non-genetic factors, such as age, disease, diet, and environment, on drug metabolism would also be detectable by this novel drug sensitivity test.”
“I hope that owners of sighthounds will not have to worry when their dogs need to undergo necessary medical procedures,” Dr. Martinez says. “The potential of being able to proactively customize drugs used for anesthesia for individual dogs to reduce the risk of slow recovery or identify a dog that is prone to a fatal bleeding problem and ensure they get lifesaving drugs is exciting.” n
Sighthound Owners Can Contribute to Research
Researchers at the Program in Individualized Medicine (PrIMe) at Washington State University are seeking DNA samples from sighthounds for two separate ongoing studies. One study is examining adverse drug reactions to anesthesia, and the other is investigating delayed postoperative bleeding. For information, go to https://prime.vetmed.wsu.edu or send an email to courtlab@vetmed.wsu.edu.
To read the abstract of the adverse drug reaction grant that is funded by the AKC Canine Health Foundation, go to: https://bit.ly/2FG1vjh. You also may donate to this research via the link.
MDR1 GENE MUTATION IN HERDING BREEDS TIED TO ADVERSE DRUG REACTIONS
The discovery in 2001 of a mutation in the MDR1 (multidrug resistance) gene in Collies and other herding breeds that causes a neurotoxic reaction to ivermectin, a parasitic preventive, provided insights into treating affected dogs. It also initiated the use of pharmacogenetics to determine how an individual dog’s genetic makeup impacts its response to drugs.
Katrina Mealey, DVM, PhD, DACVIM, DACVCP, professor and the Richard L. Ott Endowed Chair in Small Animal Medicine and Research at Washington State University, identified a 4-base pair deletion mutation in the MDR1 gene that causes a stop codon prematurely terminating P-glycoprotein (P-gp) synthesis.
“The MDR1 gene encodes the P-gp transmembrane protein that functions in a protective capacity by transporting a variety of drugs from the blood-brain barrier into the body,” explains Dr. Mealey. “Dogs with the MDR1 mutation do not have this protective barrier. Thus, drugs like ivermectin can cause toxic reactions that result in debilitating illness and even death.”
In the affected dogs, high concentrations of ivermectin accumulated in their brain tissue after a single dose of the drug. Since ivermectin is processed from the brain through P-gp into the body, Dr. Mealey hypothesized that ivermectin-sensitive collies had altered MDR1 gene expression.
Her research led to the MDR1 gene mutation discovery and development of a genetic test that is available through the Veterinary Clinical Pharmacology Laboratory at Washington State University (www.vcpl.vetmed.wsu.edu). A DNA cheek swab test that identifies a dog’s phenotype for the mutation can be ordered and processed for $60.
The autosomal dominant gene mutation impacts homozygous and heterozygous affected dogs. Dogs that are homozygous inherit two copies of the mutant allele and pass one copy of the defective gene to their offspring. Homozygous dogs are more likely to have severe, life-threatening drug reactions.
Affected dogs that are heterozygous have one copy of the mutant allele and one copy of the normal allele, meaning they have a 50 percent chance of passing the defective gene to their offspring. These dogs have less severe adverse drug reactions compared with those that are homozygous.
The MDR1 mutation primarily occurs in herding breeds. Affected dogs are thought to be descendants of a single dog that lived in Great Britain in the early 1800s before breeds were selectively bred. The mutation also occurs in two sighthound breeds, the Longhaired Whippet and Silken Windhound, believed to share a collie ancestry. Mixed breeds — any dog with a herding breed in its ancestry — may be at risk for drug toxicity.
“As a pharmacologist, the most fascinating aspect of the MDR1 gene mutation is the sheer number of drugs that are affected by a single gene mutation,” Dr. Mealey says. “Not all drugs must be avoided in dogs with altered P-glycoprotein function. Many drugs can be used safely with no need to alter the dose.”
However, adverse drug reactions involve over a dozen different drugs. The most serious adverse drug reactions involve antiparasitic preventives, such as ivermectin and milbemycin, the antidiarrheal medication loperamide (Imodium®), and several anticancer drugs, including vincristine and doxorubicin.
Since the genetic test was first offered in 2004, there has been a reduction of the mutation in some breeds via selective breeding. Importantly, identifying dogs with the P-gp dysfunction allows veterinarians to decrease the drug dose or consider alternate drugs to avoid a potentially fatal drug reaction.
Breed Frequency of MDR1 Gene Mutations1
Breed Approximate Frequency
Collie (Rough- & Smooth-Coated) 70 Percent
Longhaired Whippet 65 Percent
Australian Shepherd 50 Percent
Miniature Australian Shepherd 50 Percent
McNab Shepherd 30 Percent
Silken Windhound 30 Percent
English Shepherd 15 Percent
Shetland Sheepdog 15 Percent
German Shepherd Dog 10 Percent
Herding Breed Cross 10 Percent
Mixed Breed 5 Percent
Old English Sheepdog 5 Percent
Border Collie <5%
1Veterinary Clinical Pharmacology Laboratory at Washington State University (www.vcpl.vetmed.wsu.edu)
Drugs Affected by the MDR1 Gene Mutation1
Drug Category Drug
Analgesic/Sedative Acepromazine
Butorphanol
Antibacterial Erythromycin
Antiparasitic* Doramectin
Ivermectin
Milbemycin
Moxidectin
Selamectin
Chemotherapeutic Doxorubicin
Vinblastine
Vincristine
Vinorelbine
Paclitaxel
Antidiarrheal Loperamide (Imodium®)
*Note that giving dogs FDA-approved heartworm preventive products according to the recommended doses is safe, even in dogs with the MDR1 mutation.
1Veterinary Clinical Pharmacology Laboratory at Washington State University (www.vcpl.vetmed.wsu.edu)
Meloxicam, Proceed with Caution
The human drug Meloxicam has been routinely prescribed as an off-label nonsteroidal anti-inflammatory drug for canines. It is not without unusual but serious side-effects….
The veterinarian drug, Deramaxx, is a prescription nonsteroidal anti-inflammatory for canines to control pain and to relieve inflammation. However, the drug has experienced fluctuations in both availability and pricing. For example, at the time of this writing, 100mg tablets of Deramaxx is quite expensive. When dosing giant breeds, the usual dose of Deramaxx is 1.4-1.8mg/lb of body weight. An average weight of 150-pounds requiring relief from postoperative pain or inflammation would require almost three tablets daily. Currently, 30 tablets for a 10-day supply is $100-$150.00. If a dog requires long-term usage, 90 tablets, for a 30-day supply can cost $300-$355.00. Either amount is not spare change.
As a substitute, the human drug Meloxicam has been routinely prescribed as an off-label drug for the same purposes. Still, it is not without serious side-effects. Further, two of my Veterinarians over the years were extremely cautious utilizing the drug, and I'd go so far as to say they were reluctant to use it. I have experience using Meloxicam for at least 13 years now on our Irish Wolfhounds; however, recently, one of my Wolfhounds endured the real and severe side effects of Meloxicam. The potential side effects that both of my Veterinarians feared, and admittedly, they were very frightening.
As a preface, I do not allow the use of Opiates, such as Buprenorphine, during surgery as several years before I had a Wolfhound who suffered a severe reaction with life-threatening complications from the opiate. It may be that my Wolfhounds and, therefore, my bloodlines are susceptive to opiates. As a precautionary measure, my veterinarians do not use Buprenorphine on any of my hounds. For more information on my Wolfhound’s specific adverse reaction, please visit my Irish Wolfhound Health Concerns webpage, and scroll down to Drug Interactions. Alternatively, before surgery, we administer Gabapentin, which is a human drug that is used off-label for dogs with chronic pain relief or cancer pain. Postoperative care, we use Deramaxx and Gabapentin for pain relief and inflammation.
Again, it bears repeating that I have been using Meloxicam for 12 or more years without any incident. However, there is always a first time for everything. Kellyanne, our 5-year-old Wolfhound, had undergone surgery recently, and we agreed that she would take Meloxicam for only 4 days post-surgery to relieve inflammation. All went well while she was taking the drug, or so it seemed. Approximately one hour after eating her dinner on the 7th day, Kellyanne was resting when she began to vomit an enormous amount of bright red blood with small debris that appeared to fine in appearance, almost like coffee grinds. Her gums were pale pink, her abdomen was swelling and retaining fluid, and she was somewhat sluggish but no temperature. She then immediately developed black tarry, liquid stools, along with a lack of appetite and general weakness. The black tar stools were the fluid from her abdomen and blood from the ulcerations. Since she had ceased vomiting, the blood was absorbed and eliminated through the intestines.
As for the bloody vomit, well, I have been around a long time, and I must say that I had never seen anything quite like it. It was a frightening scene to see such excessive amounts of fresh blood pouring out of my hound's throat! SEE BELOW PHOTOS
Kellyanne was administered 2 grams twice daily of Sucralfate, which is an oral anti-ulcer drug used to coat ulcers in the gastrointestinal tract to protect them from stomach acid and allow them to heal, which were caused by the Meloxicam. Though she did not continue to vomit, it took Kellyanne five long days for her stomach to improve, her tarry black stools to disappear, and nearly seven days for the abdomen's swelling to dissipate completely. 16 days after surgery, she still is eating somewhat sparingly compared to her once normal, healthy appetite despite my medley of wonderful concoctions and treats.
I cannot stress enough to my Readers to proceed with great caution and understand the risks of using Meloxicam. Despite my long experience with the anti-inflammatory and having no previous issues, I repeat there is always a first time for everything. Kellyanne (150lbs) prescribed dose was one and a half tablets (30mg) once daily for the first two days and then one 20mg tablet once daily for the last two days, all of which wreaked havoc on her.
Eggs As a Staple In Your Dogs Diet
Eggs are a staple In your dog’s Natural Diet, but if you are not feeding a pasture-raised hen’s egg then any egg MUST be cleaned first!……
As many of you know, eggs are a major component in my hound’s "Natural Rearing" Diet. Indeed, my hounds are fed whole, raw eggs five days per week -- one egg per dog per day, as an ingredient in their VitaMix breakfast puree.
Eggs are an essential aspect of their diet, not just because of the obvious being that they are nature’s purest form of calcium. They are complete in protein and an excellent source of vitamin A, not to mention Vitamin B complexes, lethicin, and sulfur amino acids, and so forth. All of which your dog needs in their diet. Some people have worried about feeding eggs and biotin deficiencies. They point to a study with lab rats whose diet’s main staple was voluminous quantities of egg whites in which the rats developed a biotin deficiency. Perhaps this vulnerability may occur if an unknowledgeable, stupid person only fed their dog egg whites and not much of anything else. But in real life, eggs are a staple and essential aspect of any natural, raw diet. In fact, whenever they can find them, wild carnivores eat eggs as a special treat.
Not all eggs are the same!
There is a tremendous difference between commercial, factory-farmed eggs, and pasture-raised, organic eggs. There is not enough time for me to write about the significant contrasts in nutrition as Readers can perform their own research. However, pasture-raised chicken eggs are nutritionally superior to commercially farmed eggs. An interested reader may wish to review Mother Earth News study findings that the pasture-raised hen eggs contained 4 to 6 times as much vitamin D as typical supermarket eggs. Other benefits were:
1⁄3 less cholesterol
1⁄4 less saturated fat
2⁄3 more vitamin A
2 times more omega-3 fatty acids
3 times more vitamin E
7 times more beta carotene
Importantly though, the differences do not stop at nutrition and sources of origins. The other weighty, influential distinction is the bacteria commonly found on caged, factory-farmed eggs. If you are feeding commercial eggs, you MUST wash and or lightly boil them for approximately 3-4 minutes. Still, I am NOT suggesting that you feed hard-boiled or scrambled eggs to your dog! Thoroughly cleaning or gently boiling the eggs will kill the bacteria on the shells. If you do not correctly prepare them, the shell bacteria can cause canine gastric distress in the form of severe and recurrent diarrhea.
Unfortunately, several years ago, I learned this lesson the hard way, and it cost me a great deal of time and money investigating why the dogs had such constant illness. As a solution, I was fortunate to find a local farmer for fresh, pasture-raised eggs and have not had any issues since.
I advise the Reader to find a source for organic, pasture-raised eggs. If for any reason you cannot find a reputable supplier, prepare them as I said. This process includes even the "organic" eggs sold at the conventional grocery store. If you do not, the likelihood of your dog having a reoccurring illness is quite high; I can almost guarantee it.
As for color: Brown eggs versus white eggs.
Eggshell color is unique to a Hen’s breed and genetics. Diverse Hen breeds produce various colors, but supposedly, eggshell color does not change egg nutrients, only how they are raised. As the Hen forms the shell, pigments called porphyrins are secreted from the cells within the Hen’s uterus and adds color right before the egg is laid.
Why are nearly all eggs white? There are commercial breeds of chickens who have been explicitly developed for conventional egg production, one of which is the White Leghorn. This breed of Hen is used in factory-farm production complexes and lay's white-shelled eggs. Hens that lay white eggs do not produce any pigments during shell formation. Keep in mind that there are now also poultry breeding companies who have developed commercial Hen layers for industrial brown-shelled egg production, and even some being explicitly bred for pastured, poultry production. Hence, why ANY egg purchased at the supermarket MUST be cleaned or lightly boiled.
Often people ask if there is a susceptibility for white eggs to absorb more bacteria versus a brown egg. I have performed some research into this topic, and to date, I have not found any meaningful data to prove this conjecture.
To recap, if you are feeding raw eggs, make sure that you switch your supplier to one who has pasture, free-range chickens. If you live off the grid and have no available sources, then you must wash your commercially purchased eggs thoroughly BEFORE you feed them. However, DO NOT clean the eggs in advance as moisture is a threat to its shelf life.
The Ultra Fine Vitamin C Powder Out-of-Stock and Meanwhile What to Use
A quick note to share about one of two Vitamin C sources that I commonly recommend. Recently, the Ultra Fine Vitamin C Powder, Non GMO, Highest Grade of DSM's Quali-C. Pure Ascorbic Acid. 16 oz. Vegan “GMOFree Vitamins” company located in the United Kingdom were out of stock on this product. I have recommended this product in earlier Blog articles and have used it myself on a regular basis. It is one of the few Vitamin C Ascorbic Acid products NOT made in China. As I write on my Ballyhara Diet & Nutrition page 90% of all Vitamin C products are manufactured in China, and in my opinion, it is paramount that we source products NOT manufactured in China, especially edible foodstuffs.
During this outage, I used the Wholistic Pet Ester-C, as an excellent substitute which is a different form of Vitamin C being Ester-C. I recommend that you read my previous post on the pros and cons for choosing and all the particulars regarding other vitamin supplements we use. I did all the legwork for you so you might as well take advantage of it.
Read Reposting & Revised Vitamin Supplement Warnings: Look at the Ingredients!
Cardiovascular (Heart) Disease in the Irish Wolfhound
Most novice and current owners do not realize that advanced annual cardiac screenings, to include Electrocardiograms (ECG) AND Echocardiograms (Echos) are paramount in the care and maintenance of your Irish Wolfhound. Typically, these screenings are performed during the adult stages of growth (beginning at two years) and onward throughout their senior years…..
Cardiovascular (Heart) Disease
Notably, Dilated Cardiomyopathy (DCM), Atrial Fibrillation, and Ventricular Premature Complexes or Contractions (VPC).
Most novice and current owners do not realize that advanced annual cardiac screenings, to include Electrocardiograms (ECG) AND Echocardiograms (Echo) are paramount in the care and maintenance of your Irish Wolfhound. Typically, these screenings are performed during the adult stages of growth (beginning at two years) and onward throughout their senior years. However, regular electrocardiograms (ECG) are recommended earlier on to monitor any conditions that may develop. I implore all Irish Wolfhound owners to please read my DogMusings Blog Post title, "Irish Wolfhound Heart Health" for a brief but important explanation on necessary, annual, full-scale heart evaluations. Afterwards, please read the "Holter ECG Ambulatory Monitor" article for more details.
OFA Required Annual Testing
The Orthopedic Foundation for Animals (OFA) breed testing information effective April 1, 2016, states that the OFA in consultation with the American College of Veterinary Internal Medicine (ACVIM), has instituted the Advanced Cardiac Database (ACA) which has become the new standard for cardiac exams and replaced the previous OFA Congenital Cardiac Database. Moreover, all exams for the new Advanced Cardiac Database are limited to boarded veterinary cardiologists with Diplomate status in either the ACVIM (American College of Veterinary Internal Medicine/Cardiology subspecialty) or the ECVIM (European College of Veterinary Internal Medicine/Cardiology). No general practitioners or other specialists can submit examination findings.
Adult congenital clearance only remains valid for one year from the time of the exam. This is because congenital heart disease can affect our breed from early, mid to late onset ages and is why I am explicit and direct when I urge that each and every Wolfhound over the age of two should have annual, advanced heart evaluations.
Advanced heart evaluations performed by BOARD CERTIFIED Veterinary Cardiologists include:
1—An EKG, ECG or Electrocardiogram which shows electrical currents of the heart and will reveal, but not always, arrhythmia’s or abnormal rhythms.
2—An Echocardiogram (Echo) shows the physical condition and structure of the heart. One of the devastating and leading causes of death in our breed is Dilated Cardiomyopathy which essentially is the diminishment of the heart’s ability to serve as a pump. DCM is diagnosed by Echocardiography, which demonstrates the chamber dilation of the ventricles and wall thinning, and indicates, if any, decreased pump function through the heart. During an Echo the heart is evaluated in real-time, live action. This cannot be done by any other procedure. During the procedure, the Diplomate takes measurements which, in turn, they cross-reference with standard measurements for the breed to determine if they perceive a thinning of the walls, enlargement of the ventricles. If so, then the Wolfhound may be in the early stages of DCM.
ANNUAL Echocardiograms are required for the Advanced Cardiac Database and “is viewed as a critical component by the ACVIM/Cardiology group in order to even consider diagnosing dogs as normal when many cardiac diseases of concern to breeders can develop at any time in the dog’s life.”
Clinical signs of DCM occur secondary to either decreased delivery of oxygenated blood to the body (lethargy, weakness, weight loss, collapse), or to congestion of blood in the lungs (coughing, increased respiratory rate and/or effort, abdominal distention) or both. Cardiac dilation, decreased oxygen supply, and increased oxygen demand secondary to elevated heart rate and ventricular wall stress may predispose to the development of cardiac arrhythmia’s arising in either the atria (atrial fibrillation, supraventricular tachycardia) or in the ventricles (ventricular premature complexes, ventricular tachycardia). Arrhythmia’s may predispose affected dogs to sudden death.
Unfortunately there are far too many IW owners who think they know-it-all and assert that their local veterinarian listened via auscultation (Stethoscope) to the hounds heart and no arrhythmia’s were detected. Even worse, there are general veterinarian practitioners who believe that EKG’s will suffice and that the odds of an Echo or further, a Holter monitor diagnosing any arrhythmia without an irregular EKG is essential lay impossible and therefore contraindicated. Straightforwardly, no Diplomate would agree with this notion. Simply because an EKG does not reveal aberrations does not clear the hound of arrhythemia’s, DCM, abnormalities of the pericardium, possible tumors, blood clots, etc.. ONLY an Echocardiogram can do so.
Negligent treatment by unknowledgeable general Veterinarians are risking the well-being of many companion wolfhounds and I implore the owners to be their Wolfhound’s health advocates. Ask questions, disagree, schedule the annual Advanced Cardiac Assessments yourself with a Board Certified Cardiologist. If you have to drive several hours each way — so be it! Trust me when I tell you that doing so may SAVE your IW’s life in the future as well as a world of heartbreak.
If the Board Certified Specialty Practice requires referrals then advise them that you do not have one as you disagree with your general veterinarian about the advanced cardiac screenings your HIGH RISK BREED requires. Repeat what I have stated above and inform them that the Advanced Cardiac Database (ACA) has become the new standard for cardiac exams and that all exams for the new Advanced Cardiac Database are limited to boarded veterinary cardiologists with Diplomate status in either the ACVIM (American College of Veterinary Internal Medicine/Cardiology subspecialty) or the ECVIM (European College of Veterinary Internal Medicine/Cardiology). Keep in mind that you are not required to submit any findings to OFA.
Lastly, consider that as part of the Advanced Cardiac Database both the Boxer and Doberman breeds are required to submit Holter Event Monitor results (24-hour ambulatory EKG) in addition to Echo & EKG. If the annual gold standard for Boxers and Dobermans includes Holter Monitor results then it should be the gold standard for Irish Wolfhounds as well.
It is my considered opinion that annual heart testing on all adult Wolfhounds, from two years onward, should include an annual Holter ECG Monitoring which is a 24-hour recording to monitor for irregular heart rhythms. Undiagnosed or unknown malignant VPC's can result in feinting, collapse (syncope) or worse, sudden cardiac arrest.
I will be straightforward, if you desire this breed then you must be prepared for the expenses that come with them, and at the risk of sounding crass, you need a fat wallet. Yearly cardiac evaluations can cost, depending on your region, $400-$750 per a Wolfhound. If your Irish Wolfhound is diagnosed with cardiac disease, pharmaceutical expenses for their heart health management can be costly as drugs regularly increase in cost. The annual costs for cardiac drugs will outweigh any annual cardiac screenings with a Board Certified Cardiologist. Parenthetically, the drugs used for treating heart conditions are the same ones used for humans. See my Expenses page.
As a disclosure, I must state though that I do not concur with the statement set forth on the Irish Wolfhound Foundation website suggesting that we have experienced a decrease in overall heart conditions in our breed. I especially disagree with the suggestion that VPC arrhythmia's are mostly benign in Irish Wolfhounds. In my considered opinion, numerous hounds have or develop malignant ventricular arrhythmia's and these can be diagnosed by comprehensive annual heart health exams and controlled early on with life-saving, and life-prolonging drugs. I have received too many inquiries and calls from people looking for a puppy or advice who had lost an IW to heart disease or who have an IW diagnosed with such and the hound is faring poorly. I always inquire as to when the heart condition was diagnosed and 100 percent of the time the owners informed me that it was recently diagnosed and all said they had NOT had ANY advanced annual heart screenings performed on the wolfhound prior. Not one. The reality is that people do not take responsibility and educate themselves about the breed of dog that they have and are then heartbroken when a chronic, manageable disease is diagnosed at too late a stage.
The Wolfhound cannot be his own Health Advocate!
Irish Wolfhound or Any Sighthound Breed Emergency Kits
I suggest that all Irish Wolfhound owners organize and have an emergency kit available at all times, especially if you plan on traveling with your Wolfhound. In it should be several indispensable items that I have linked to Amazon for ease of purchase….
I have posted on my website Irish Wolfhound Health Concerns the items that are absolutely necessary for an Emergency Kit. This kit is terrific for any of our Sighthounds but could be a lifesaver. If anyone has additional suggestions please send me a comment or an email.
Irish Wolfhound Emergency Kits
I suggest that all Irish Wolfhound owners organize and have an emergency kit available at all times, especially if you plan on traveling with your Wolfhound. In it should be several indispensable items that I have linked to Amazon for ease of purchase. Just click on each item’s photo following the list.
Hyland's Carbo Veg. 30X Tablets, Natural Homeopathic Relief of Nausea, Heartburn or Gas. IMO, these Carbo Veg pellets are crucial to have if you own any giant or breed prone to Bloat. If your wolfhound is pacing, looking very uncomfortable, has difficulty lying down or lies down and immediately gets up or is retching and or vomits yellow bile, or has a firm, distended stomach then dose immediately with the adult human dosage of 4 pellets. However, if you have a very large IW weighing approximately 160 pounds or more then I would begin with 6 pellets. Tip 6 pellets into the bottle cap and then raising his muzzle upwards, open your IW’s mouth and drop the pellets into the back of their throat, quickly closing his mouth and massaging his throat. If they are not swallowing or trying to gag grasp the muzzle closed and then blow in his nose to make them swallow. The pellets dissolve within a 20-30 seconds. Repeat again every 30 minutes while you seek emergency medical care.
Alumina from Boiron 30c. This is another important homeopathic remedy that is in my Emergency Kit at all times. Boiron® indicates that Alumina may be effective in alleviating various digestive issues. Aloe in this form could provide relief from stomach problems‚ like flatulence and indigestion. I use this the same exact way I use the above Carbo Veg. and dose immediately after I dose with Carbo Veg. I recommend using the adult human dosage of 5 pellets, but again if you have a very large wolfhound over 160lbs. then I would increase to 6 pellets. Repeat again every 30 minutes while you seek emergency medical care. Both of these homeopathic remedies may alleviate the gas buildup causing distress and could very well save a life while you are seeking emergency care, and may relieve or reduce the gas buildup while you are en route to a Veterinarian.
Remedies for simple upset stomach. If your dog has an upset stomach, the above recommended Carbo Veg and Alumina should be used to quell the nausea. For non-emergencies, use the Carbo Veg and Alumina 4 times per day if your dog is nauseated, car sick or is refusing food and they do not have a temperature.
Metronidazole aka Flagyl. We do not travel with our wolfhounds without bringing along prescription Flagyl. It is an antibiotic that treats diarrhea resulting from inflammation of the colon due to bacteria, as well as intestinal infections due to the Giardia parasite, Gastritis and Colitis to name a few. This you will have to obtain from your Veterinarian as it is only available via prescriptions. Get a bottle before you leave.
Proviable DC Digestive Health Supplement. This is a portable Probiotic with Prebiotics that should be given when a dog has diarrhea. Each Capsule has 5 billion CFU’s. However, I give this on the day of our trip and every subsequent day afterwards while traveling until we return home as it regulates the Ph balance in the gut and is very helpful during times of stress. Dosage is one capsule daily during times of travel and is easily hidden in a soft treat. Give immediately at the first signs of loose stools.
Rectal Digital Thermometer.
Gauze, non-stick bandages, and adhesive tape. This is for covering a wound, stopping bleeding or even a sprained ligament. I use 3M Vetrap 4” wide, soft gauze and nonstick gauze pads. Also stock waterproof adhesive tape, especially if it is wet outside as Vetrap is not waterproof.
A Canine First Aid Manual and/or download The American Red Cross App “PET FIRST AID”. Have either or both available at all times —I recommend “Dog First Aid: A Field Guide to Emergency Care for the Outdoor Dog” which is pocket sized and can fit in any emergency kit. The American Red Cross App PET FIRST AID is very good as well and is on my Smartphone and iPad. Another choice for a small portable emergency book is the Pet Emergency Pocket Guide 2nd Edition which has tabs at the bottom making it very easy to find information in a hurry.
Cephalexin Antibiotic. I do not travel without this antibiotic in case of the onset of high fever which may be present if the Wolfhound has diarrhea or lethargy. You will need to obtain Cephalexin from your veterinarian as it is a prescribed antibiotic. Explain that you will be traveling with your hound and in case of emergency, away from home, it may be extremely helpful to control an unexplained fever as a result of a bacterial infection such as a respiratory tract infection or a soft tissue infection.
Dog Ear Wipes. Such as VetWELL Dog Ear Wipes - Otic Cleaning Wipes for Infections and Controlling Yeast, Mites and Odor with Aloe and Eucalyptus.
Cotton Balls and Swabs. I carry the long ear swabs such as BambooStick Cotton Buds for Dogs for hard to reach spots deep in the ear canal.
Scissors.
Bottled Water. Always, always, always use bottled water or bring enough water from home to last the duration of your trip. Do not give your dog water that he or she is unaccustomed to as it could result in diarrhea.
Multiple Organ Failure and Acute DIC
Sadly, we lost our much loved Danny several weeks ago at 9 years 11 months of age. Though we did not perform a post-mortem, the suspected cause of death was multiple organ failure and possibly acute DIC (disseminated intravascular coagulation)…..
Lisa and Ballyhara Danny 2018
Sadly, we lost our much loved Danny several weeks ago at 9 years 11 months of age. Though we did not perform a post-mortem, the suspected cause of death was multiple organ failure and possibly acute DIC (disseminated intravascular coagulation). My primary vet believed it to be Hemorrhagic Gastritis as it had a very sudden onset with black tarry sludge pouring out of him. This color is caused by iron in the blood becoming oxygenated when it passes through the ileum and colon. One minute he was healthy, running around the paddock and he came into the house to rest, slept soundly, and when I entered the room again, he had just gotten up and had black sludge flowing out of him. I had never seen anything like it and can best describe it as turning on a faucet. There was no vomiting, and his gums were very pale. The quantity was so vast that I had to hose the lawn down where the black coal revealed itself as blood with a foul odor. Danny was rushed to the veterinarian, and we ran bloodwork diagnostics on him. His red blood cell count was low, and his white blood cell count was very high. Generally, with Hemorrhagic Gastritis, the red blood cell PCV (Packed Cell Volume) is elevated and often they have normal or low blood protein levels. As a result, this diagnosis was set aside. My gut feeling was that an organ(s) was shutting down as a result of the heart medications and nerve pain medication he had been taking over several years, on a daily basis. He had been taking 1500mgs of Mexelitine 3x daily; 80mgs Sotalol 2x daily; Pimobendan 40mgs daily; Enalapril Maleate 40mgs daily; Gabapentin (for his Cervical neck injury see other posts) 400mgs 2x daily.
Ballyhara Danny
I must deviate here to point out a relevant topic. All novices and students of Sighthound breeds should be acutely aware that CBC (complete blood counts) and blood chemistry as related to Sighthounds, in general, are different than other breeds. Typically, Sighthounds have WBC (white blood cell counts) values usually at the very low end of the normal range. So, for example, IDEXX Laboratories values state that average WBC counts (Reference Interval) are 5.05 to 16.76. Danny's was 17.23 which indicated either extensive inflammation, infection or other stresses. Typical Sighthound WBC should range from 5-6, and everyone should be aware of this idiosyncrasy. If their sighthound's WBC is elevated above this 5-6 range then, indeed, a WBC of 8 is considered raised for this genre of dogs and should be of concern.
Even if my gut feeling were correct, there would be no hope for Danny, but my vet wanted to proceed if he had a massive infection, though he had no temperature. We started with an injectable Baytril along with an intervenous dosage of Metronidazole (Flagyl), and IV fluids over the course of several hours after which I brought him home. That early evening as he relaxed in the shade on the patio he again had a small amount of black stool leach out of him. I take great care in making sure that my hounds are well-hydrated; therefore, I gave Danny an organic low-sodium warm chicken broth (8 ounces to start) via an oral syringe to provide him with energy and nutrients. The next morning, I began organic baby food purees such as simple chicken and rice along with small amounts of applesauce and yogurt but he would not freely eat it, and I had to hand feed it to him. This was entirely out of the ordinary as in the past when he had a bout of diarrhea after picking some virus up at a dog show he would still freely eat food if it were offered to him.
Note: On the topic of diarrhea and fasting, I DO NOT subscribe to the notion of fasting a dog who has diarrhea. I especially do not Fast an Irish Wolfhound, even more, a 10-year-old male weighing 173 pounds (without an ounce of fat on him!). Many of today's mainstream vets still recommend fasting the animals for 24 hours. Nonsense I say, as this only enhances the misery, it weakens them further and makes them feel even crummier. More shamefully, some Internet columnists recommend no water which is dangerous as diarrhea causes dehydration and the loss of electrolytes. Also be aware that there are one or more studies that show that Microbiota modulation changes occur due to a negative impact on gut physiology from fasting. The loss of microbiota is very concerning, and in my considered opinion, it is JUST ONE of several determinants in Gastric Torsion or Bloat (I have no data to prove this, but it has been a theory of mine for decades). Additionally, I also give raw honey -- NOT honey purchased in a supermarket but unheated, unprocessed raw, pure honey.
Despite my efforts, it was evident to me that a much more serious underlying issue was occurring. Though Danny's gums regained some color, they remained paler than usual and his Capillary Refill Time was prolonged. Though he was not lethargic and lying on his side, he still remained in the prostrate position up on his elbows which is another sign that seasoned breeders look for depending on the issue we are attempting to detect or determine. He had fight in him, but he was not interested in the food I was giving him which again was remarkable for him. The end of the third day brought no improvement, despite his antibiotic regimes as he, again, had small amounts of the black coal leaching out of him where he lay. By the morning of the fourth day Danny still had black feces coming out of him, albeit in much smaller amounts, and still had no interest in food. It was then that we knew that we had to help him pass on as fluid began accumulating in his abdomen.
Here I must tell the Reader as to how Danny chose to pass on because it was quite extraordinary. At 10 years of age, Danny had always been very astute and had learned that unfortunately on a few occasions, our longtime primary veterinarian's appearance at our home coincided with the loss of one of our wolfhounds. I have always insisted that my hounds leave while at our home where they are comfortable and not frightened. Over the 10 years of his life, he had noted the loss of litter sisters, as well as his Dam and Uncle, and his partner Jane. He also learned very early on to identify our veterinarian's car so that in the past, whenever Darcy arrived for annual exams, blood draws, Rabies vaccinations or Titers, even before she exited the vehicle, he would bark at her with an unusually high pitch. A bark that was nothing like how he barked when a stranger arrived, or at the neighbor's dogs when they walked by the house, or while trying to play with the other hounds. On the 4th day, as Darcy arrived for the euthanasia, we were outside in the garden that he loved, resting on a blanket as he was up on his elbows, and as she drove in the lower driveway, he watched her carefully and silently. He did not attempt to bark, he did not try to raise himself up to greet her, just silence. It was not because he was weak or sickly as he lay there proudly arching his neck with the most magnificent gaze while watching her enter through the gates to examine him. He simply knew it was his time to leave us. He was not frightened, but instead, he was ready. And as he looked me in the eyes for the last time, he licked me and said farewell and was gone within a few brief seconds. He was a remarkable animal, and my exceptional friend, one I will never forget.
Danny died 4 weeks short of 10 years of age and 10 days before his grandchildren being born. We would have loved for him to have been able to be here for his grandchildren as we have Danny's mate and the pups Grandmother, Kennedy, still with us who is 10 and a half years of age. I firmly believe that the organ failure was due to the extensive medications he was taking for his late onset, adult Ventricular Tachycardia heart disease, without Dilated Cardiomyopathy. He had undergone a final echocardiogram four months earlier as well as a 24-hour ambulatory Holter monitor in which the Cardiologist had increased his Sotalol to 80mgs 3x daily. Some forms of heart disease are considered a chronic disease in which some dogs can live for years on medications, but there are consequences to this. I believe there are long-term effects from the drugs that develop over time and can result in organ failure.
Ballyhara Cinneide (Kennedy) 10 yrs 4 months with grandpup
Amicar and Post-Operative Bleeding in Irish Wolfhounds
Irish Wolfhounds bleeding-out after surgery and untimely deaths. Amicar is a drug that is strongly recommended for ALL Gazehounds for use immediately following surgery!
Within the Ballyharaiws.com website, I have an entire section dedicated to Irish Wolfhound Health Concerns along with Spay Neuter Concerns, in which both contain essential recommendations and precautions all Wolfhound owners should take BEFORE any elective surgery on their Sighthounds. You will find reports about the Greyhound and Scottish Deerhound authored by John Dillberger, DVM on the dangers of Post-Operative bleeding in Sighthounds and the drug that should be administered immediately following any surgery.
In the late 2000s, disproportionate cases of postoperative bleeding were taking place in Greyhounds one or two days after surgery in which affected dogs formed normal blood clots but then dissolved too quickly resulting in early deaths. Foremost, in the Greyhound studies, Blood Clotting Function was tested before surgery, and results were normal as were their Serum Chemistry Profiles and Complete Blood Cell Counts.
Aminocaproic Acid (Amicar) is a drug vital to Sighthounds most often when you least expect it such as after routine spay neuter surgery or more complicated operations in areas prone to more profuse bleeding. The drug prevents or treats delayed postoperative bleeding usually given every 8 hours for five days. Without having taken Amicar, I know of at least two Wolfhounds who, after surgery, one or two-days later "bled out" and died and their blood clotting tests, CBC, etc. were also normal.
According to the report, Gazehounds with high-performance circulatory systems have thick blood moving at high speed and under high pressure. Consequently, they have more frequent blood vessel damage and micro-clot formation. As a consequence these Gazehounds almost certainly have fibrinolysis systems that are hyperactive, putting them at risk for delayed
postoperative bleeding. The clots form but begin to dissolve far too early leaving the hound in jeopardy. Typically, the hound goes home with the owner, but complications begin approximately 24-36 hours later, and hounds have been found dead having bled-out.
The Board Certified veterinarian I spoke with explained that they believe it is a recessive genetic mutation which you CANNOT possibly know exists, regardless if "You have never had it before." Remember, each of your hounds do not inherit the same genes as the other another from each Parent. It is possible that one littermate may inherit such mutation associated with high-performance circulatory systems and another does not but one thing is certain, you can never be sure. Do not risk not using Amicar, otherwise, you could wake up one day to find your beloved companion has died.
Keep foremost in mind that Amicar is a SPECIALTY drug that most veterinary practices do not usually have in stock unless they are a specialty clinic. As such, Amicar MUST be ordered in advance and kept on hand at your local facility in case of an emergency such as Bloat surgery, and it is 3:00 in the morning.
Recommended Heartworm Preventative for Irish Wolfhounds & Sighthounds
Heartworm preventative recommendations for Sighthounds by Dr. W. Jean Dodds, DVM, is and has been available via her popular Pet Health Resource Blog. If you missed it -- here is the abbreviated info from her "Quick Guide to Heartworm Preventives."
Heartworm preventative recommendations for Sighthounds by Dr. W. Jean Dodds, DVM, is and has been available via her popular Pet Health Resource Blog. If you missed it -- here is the abbreviated info from her her article "Heartworm: A real and present danger"
I took parts from the section "Quick Guide to Heartworm Preventives" to share with Sighthound fanciers.
- Foremost, I recommend administering heartworm preventive every 45 days instead of every 30 days, but only if this interval is strictly adhered to and if it’s difficult to keep track with a reminder calendar, then your dog may need to stay on the medication every month.
- Animals that have been taking monthly preventives for a relatively long time may develop subsequent product intolerance. Other preventatives should be sought out or rotated (Please see her blog and other articles for more details on alternatives).
- Dogs affected with autoimmune diseases and their immediate relatives should receive only plain daily heartworm preventive (Dimmitrol = diethylcarbamazine). This drug can be found in Canada. For more information about dogs who have autoimmune diseases, chronic thyroid or liver conditions, please visit my blog post, “General Recommendations for Heartworm Preventives.”
- Trifexis is an oral preventative for fleas and heartworm. Trifexis contains spinosads which are contraindicated in epileptic or seizure prone dogs and should not be given to these dogs. Unfortunately, this is generally unknown and should be shared with your veterinarian, friends and family.
- Plain milbemycin oxime (Interceptor) is preferable as a heartworm preventive for certain groups of dogs, like sighthounds, smaller white breed dogs and those prone to seizures. (My bold font)
For my Wolfhounds, I now use Interceptor as my preferred brand of heartworm preventative and I administer it every 45 days throughout May to December.
Autoimmune Diseases and Heartworm Preventatives
As of late, we have been learning of Irish Wolfhounds afflicted with autoimmune diseases. For those who are unfamiliar, do not feel left out as up until the past two decades autoimmune maladies were somewhat exotic. Not any longer. We now hear of alarming incidences of dogs with an autoimmune disease, particularly in Irish Wolfhounds throughout the country. What does this have to do with heartworm preventative?
As of late, we have been learning of Irish Wolfhounds afflicted with autoimmune diseases. For those who are unfamiliar, do not feel left out as up until the past two decades autoimmune maladies were somewhat exotic. Not any longer. We now hear of alarming incidences of dogs with an autoimmune disease, particularly in Irish Wolfhounds throughout the country.
Autoimmune diseases are caused by the immune system attacking itself triggered either accidentally or by infection or another illness. Quoting Ernest Ward, DVM at VCAhospitals.com, "Autoimmune disease can affect a single system or multiple body systems. Autoimmune diseases can affect skin, connective tissues, nerves, muscles, the endocrine system (the system that controls hormones and other chemicals), red blood cells, and the digestive system."
Usually, the most recognized symptom of an autoimmune disease is skin problems, and they can be very complicated. A few examples that Dr. Ward discusses are:
Bullous Pemphigoid
Systemic lupus erythematosus
Discoid Lupus Erythematosus (DLE)
Pemphigus complex of which Pemphigus itself is a group of five autoimmune skin separate diseases. The Reader can do further research at VCAhospitals.com.
However, there seems to be no limit to the damage autoimmune diseases can inflict. According to Dr. Jean Dodds, DVM, who has written extensively on these subjects throughout the decades, autoimmune diseases affect the thyroid, blood, eyes, skin, muscles, joints and specific organs.
Most prominently, besides skin diseases, is the digestive system. It is one of the most commonly affected organs in which Irritable Bowel Disease, and Leaky Gut Syndrome or Intestinal Permeability occurs. See my Nutrition and Health Concerns pages about Leaky Gut Syndrome.
What does all this have to do with heartworm preventative? If your hound is suspected or diagnosed with an autoimmune disorder, then they should not be vaccinated! However, just as important is the type of heartworm preventative that can or cannot be used. Even more, the kind of Heartworm Preventative will vary depending on what breed of dog you have as well!
As Dr. Jean Dodds explains in her article, "Dr. Dodds’ Take on and General Recommendations for Heartworm Preventives"
"Some individual animals affected with autoimmune diseases and their immediate relatives have been shown to react adversely to commercial, monthly heartworm preventives. When an individual’s immune system is compromised, any regular exposure to particular kinds of drugs, chemicals or toxins can produce significant adverse effects, whereas these exposures are well-tolerated by animals by animals with healthy immune systems that do not carry the genetic susceptibility to these disorders. It is important to emphasize that the licensed drug or chemical is safe unless used in a genetically or physiologically susceptible companion animal. These adverse reactions usually occur within the first 10-14 days after the monthly product has been administered and typically begin after an animal has had 2-5 doses. Occasionally, animals that have been taking monthly preventives for a relatively long time will develop subsequent product intolerance. This usually indicates that some underlying disease process has emerged to explain the problem. Based on cumulative data, it is my recommendation that dogs affected with autoimmune diseases and their immediate relatives receive only plain daily heartworm preventive (Dimmitrol = diethylcarbamazine). If heartworm disease is not prevalent where the animals live, routine use of heartworm preventives is not recommended. This is especially important for dogs suffering from chronic diseases of the skin, hair and coat, or those with bone marrow, thyroid or liver disease."
It is vital that an autoimmune disease be diagnosed as quickly as possible as the severity of the symptoms can be severe and complex, meaning they can consist of multiple parts which will always complicate matters. Keep your spirits up; although autoimmune diseases cannot be cured unless they are caused by environmental factors that can be diminished or eliminated, most times, with a concerted effort, these diseases can be controlled.
Canine Nasosinal Tumors: In Memorium To Declan
Declan's Nasosinal Cancer.
Well, with Declan I first noticed that she was favoring eating her chicken wings on the left side of her mouth. I thought it somewhat odd but decided just to watch her for a day or so as I checked her lower jaw but did not notice anything. Then this favoring advanced to her eating her wings much more slowly which was definitely out of the ordinary as she was a voracious eater. Within two days, Declan began to go down fast developing a fever of 103.9. I made an emergency appointment with our soft tissue veterinarian surgeon and was fully prepared to have her anesthetized for a thorough mouth exploration.....
It was great sadness that we had to bid farewell to our glorious Declan at nine years eight months of age. I was so looking forward to having four ten-year-old wolfhounds in my home, but alas, it was not meant to be. It came as even more of a surprise as Declan had always been extremely healthy and she would have been the last wolfhound I would have expected to leave us.
Ballyhara Declan
Declan was euthanized due to advanced nasosinal cancer. This disease was a first for me in my nearly 35 years of immersion in this majestic breed. In the end, she was glad to go, but she fought like hell to survive in the weeks leading up to her passing.
I have always stressed to anyone who would and will listen that the Irish Wolfhound breed is too damn stoic. Far too stoic and, in my opinion, this stoicism jeopardizes their lives. In this particular case, though, there was not much else we could have done, and I did all that I could do. In other situations not involving terminal illnesses, the only way to combat this stoicism is increasing our vigilance for even the smallest change in behavior. In doing so, we may head off a quickly downward spiraling illness that could take the life of our beloved companion.
Declan's Nasosinal Cancer.
Well, with Declan I first noticed that she was favoring eating her chicken wings on the left side of her mouth. I thought it somewhat odd but decided just to watch her for a day or so as I checked her lower jaw but did not notice anything. Then this favoring advanced to her eating her wings much more slowly which was definitely out of the ordinary as she was a voracious eater. Within two days, Declan began to go down fast developing a fever of 103.9. I made an emergency appointment with our soft tissue veterinarian surgeon and was fully prepared to have her anesthetized for a thorough mouth exploration. However, when we arrived our veterinarian examined her lower mandible and molars (Declan was very stubborn about having her mouth opened wide, and now we understand why) and noted her gums were bleeding. His immediate thought was that she had inflammation of the gums due to an infection which most likely was the cause of her fever. As such, he prescribed Cephalexin which has always been an excellent antibiotic, and I have had excellent results using it.
While on the Cephalexin, she did not improve and was eating very poorly plus she now had blood seeping from her mouth. We returned to our veterinarian immediately in which this time she was anesthetized so we could ascertain the cause of the problem. Once on the table, my vet rushed back to inform me that Declan had a large hole in the hard palate of her mouth near the upper right molars, and moreover, the four rear molars were so loose that one could move them with a finger. I hurried to witness the damage myself and was utterly aghast. How could this wolfhound even attempt to eat with such an open wound in her mouth? How was it she was walking around for that matter? I was stunned at the sheer stoicism of this noble animal in front of me lying on a surgical table. Of course, the only thing to do at this point is to repair the hole, but we could not close it entirely due to the massive infection, and therefore, a small section was left open for it to drain. Also, the four upper molars were removed, and a biopsy was performed including margins around the dead tissue. While we waited for her to become conscious, my veterinarian and I discussed the possible causes of this hole.
We discussed cancer as a definite possibility, but because of the proximity of the hole right next to the upper molars, it appeared that it most likely was caused by a bone. More specifically, a beef neck bone as the shape of a beef neck bone could allow for impairment in this unusual location. It was odd that the hole was not in the center of the hard palate or nearer the front of the upper jaw. My veterinarian has seen both bone injuries in other patients as well as nasal carcinoma, and it was his opinion that this case appeared to align itself more towards damage from a bone.
At this time we should have performed Nasal Radiography, but we did not as my vet believed that the results would be obscure due to the complexity of the anatomy of the skull and nasofacial areas. These include the sinuses, mandible, cavities, dental arcades, and subsequent shadows, lines, and ossifications. Looking back, I should have insisted so that I could have saved Declan from further suffering. However, at this time, the information presented to me supported the notion that this was a recoverable illness and I have regularly gone to heroic efforts to give my Irish Wolfhounds every opportunity and a chance at life, even when diagnosed with a mostly terminal diagnosis, excluding amputation and radiation therapy.
We then initiated a more aggressive antibiotic protocol of Baytril and Clavamox for 14 days. Amazingly, Declan's appetite improved the same day of surgery and later that evening while home she had a very healthy dinner. But, that did not last. What followed were strange breathing and coughing noises that sounded to me as if she had aspiration pneumonia. Accompanying this were sneezing and mucus discharge from her right nasal cavity. Despite that Declan was scheduled to undergo anesthesia to close the small gap previously left open for drainage seven days after the initial surgery, we were concerned and brought her back four days later for a re-check. Our veterinarian saw healthy, pink tissue surrounding the small opening left open for drainage. This evaluation was both positive and uplifting, and we thought that if I could eliminate the harsh breathing or what I believed to be a respiratory infection, then she would recover fully. The biopsy came back indicating extreme inflammation but could not rule out carcinoma. Seven days after the first surgery, Declan was again anesthetized, and the remaining opening closed.
As we finished her second drug protocol, this harsh, noisy breathing did not dissipate. The green mucus was appearing out of both nasal cavities now, and her right eye was weeping. Parenthetically, during my research, I discovered that this harsh breathing is a common symptom of nasosinal cancer technically called stertorous breathing. Still believing that we were dealing with a massive nasal infection and aspiration pneumonia as both illnesses have very similar symptoms, I investigated other drug protocols. I immediately thought of utilizing Rocephin. However, it presented too many challenges for obtaining it. I came upon a new 2017 Journal of Veterinary Internal Medicine titled "Antimicrobial use Guidelines for Treatment of Respiratory Tract Disease in Dogs and Cats," in which the scientists recommended treating Pneumonia with or without sepsis with Ciprofloxacin and Clindamycin. We began a new antibiotic protocol, but despite the new drugs, the green mucus now contained blood.
Declan did not improve, and we once again returned to the veterinarian's office and performed digital radiography on her lungs and throat and discovered an area tucked up in the left lobe of her lung that was implicative of infection. There were no tumors present in her lungs, and her throat radiography did not reveal any abnormalities. I decided that no more oral antibiotics were going to be administered and we used, as a last-ditch effort, an injectable medicine "Convenia" that lasts for 14 days. It is an antimicrobial drug indicated for the treatment of infections caused by susceptible strains of Staphylococcus intermedius and Streptococcus canis. Our consulting veterinarian specialists concurred, however, my hope had faded at this point as we were able to pry open her mouth to find a small hole that had reappeared.
It was now clear that it was a neoplasm and Declan was suffering. Shortly after she was euthanized at home and immediately after my veterinarian and I opened her mouth wide to observe that the one small hole had developed into at least two to three large holes in the hard palate of her mandible. After her death, I made some promises to myself. Although conservative actions are appropriate in many cases while dealing with diagnoses in Irish Wolfhounds, I regret not being persistent on obtaining a nasal radiography that may have revealed the tumor whether it was in her frontal sinuses or nasal cavity. If I had done so, I would not have allowed this magnificent creature to endure on the antibiotics regiments.
In closing, I firmly believe Declan's cancer could or would have presented itself with even more severe symptoms such as facial abnormalities or significant distant spread (metastasizing) if it were not for the Systemic Enzyme protocol she and all my wolfhounds receive, on a daily basis. I have been a proponent of regular systemic enzyme consumption for combating inflammation, regardless if it were from arthritis, cancer, injury, panosteitis, skin & coat conditions, autoimmune diseases, and age. Systemic enzymes such as Vitacost.com Flavenzyme or Garden of Life Wobenzyme are two of the best brands available (See Below). Most importantly, these are given on an empty stomach at least 1 hour before food.
Consider even more benefits of systemic enzymes, as I quote Mary Straus of The Whole Dog Journal July 2012 Issue,
"Studies in the U.S. are limited, but systemic enzyme therapy has been studied and used in Germany for decades. For example, a 2008 German review (http://www.ncbi.nlm.nih.gov/pubmed/19116226) of “rigorous clinical studies” published in the journal Integrative Cancer Therapies found that “systemic enzyme therapy significantly decreased tumor-induced and therapy-induced side effects and complaints such as nausea, gastrointestinal complaints, fatigue, weight loss, and restlessness and obviously stabilized the quality of life. For plasmacytoma patients, complementary systemic enzyme therapy was shown to increase the response rates, the duration of remissions, and the overall survival times.”
Split Tails
A common search phrase on my website is happy or wagging tail injury. A frequently seen injury in Irish Wolfhounds, we refer to it as split tails and the injury can be very problematic to care for until it heals completely. I have this information on my Health page website, however, here it is as a convenience for those who are reading my Blog.........
A common search phrase on my website is happy or wagging tail injury. A frequently seen injury in Irish Wolfhounds, we refer to it as split tails and the injury can be very problematic to care for until it heals completely. I have this information on my Health page website, however, here it is as a convenience for those who are reading my Blog.
Trauma:
A common problem in the wolfhound breed is tail damage. Typically, tail damage occurs when the hound swings the appendage too hard severely bruising and even splitting the tail open. For those experienced with wolfhound "split tails," it often can be a nightmare. It looks like a murderous crime scene as the blood is flung near and far over furniture, ceiling, walls, drapery and the like. The excited hound gets even more excited as one or more owners are trying to grab the tail and the hound at the same time to place bandaging on it to stop the bloodletting!
New owners are shocked but stay calm as there are some solutions, but they are going to require effort and diligence. First, a bleeding tail is a challenging area to keep bandaged and especially hard to heal thoroughly so that the affected portion does not open up again in another future incident, which by the way, I guarantee will happen again if not completely healed the first time. Unfortunately, as often is the case, split tail injuries on a happy, excited wolfhound do not always heal without another incident taking place. If you have bred Irish Wolfhounds long enough, then you have or had, at least once, a wolfhound with a split tail.
Again, you must understand and be prepared for the fact that a lower tail injury is a hard place to heal, and, therefore, the area will remain susceptible to further insult and injury. Scar tissue must develop over the injured area before you can ever claim victory. It can take as long as two to three weeks for the damaged tail to heal ONLY if properly cared for, and only if it does NOT receive further and ongoing damage. If the location is repeatedly damaged, then the last resort is to amputate the portion of the affected tail.
What To Do:
To begin; DO NOT wait to treat the wound as this will be your biggest mistake. Skin infections and self-mutilation will usually always occur because more often than not the dog will begin to lick and chew on it as it can be painful or itchy. This will lead to infection.
There are some "homemade" solutions out there on the Internet, and it can be a trial and error process depending on the personality and behavior of your Wolfhound. Foremost, bandaging the tail can be very tricky, and you need the correct items plus an owner must be cautious not to wrap too tightly thereby cutting off the blood supply. Bandages need to be frequently changed to prevent infection. Other variables include:
1-Will your hound leave the bandage and splint on without chewing it off?
2-The hound allows the bandage to remain, but he still wags his tail so hard that despite being cushioned and wrapped; it bleeds inside the wrapping. Subsequently, if the dressing is not changed daily, the wound will remain wet and become infected!
3-Thus, the other dilemma is how do you keep the tail wrapped? But in many cases it must also be secured somehow to the body so that it is not freely hitting objects and furniture when the dog wags their tail again yet allows the dog to raise it to defecate.
First things first:
Medical Care & Bandaging. There are so many different products on the market to promote healing of a chronic hemorrhaging tail wound but there seems to be a consensus for the basics. To start, most agree that a wound cleanser such as SAF-Clens® AF Dermal Wound Cleanser be used first and/or a Hydrogel dressing, such as Hollister Restore Hydrogel, be applied before using sterile primary bandages. SEE BELOW for the links are included to the products within this article.
Remedies:
One novel approach to resolving split tails is called Dog Ends created by a company called Bonovate. Sold by Jorgensen Labs here in the U.S., it is a new approach to solving the age-old dilemma of how to get the tail to heal with fresh air circulation but protecting the delicate area so that it is not opened up again. Check out the photo of the product below. Dog Ends dressing are open-mesh construction that allows for protection of the area while permitting fresh air to heal the wound but redirecting impact from the injury. In the beginning, the tail may be very painful and inflamed and the dog may cry out if you try to wrap it so you should speak with your veterinarian to possibly have a course of antibiotics and a pain reliever subscribed for the dog. Then the area needs to be wrapped.
Review the sites that I provide here such as Vetruus.com and the two videos provided by Jorgensen Labs. If you choose this therapy READ THOROUGHLY and follow directions! Remember, bandages need to be changed regularly. This interesting solution is recommended in conjunction with a collar that does not allow the dog to turn and chew at the tail and rip off the netting. Collars such as the one included below, KONG Cloud E-Collar, are good alternatives for preventive use.
An old idea that I used several times in the past were Duct Tape and Tube Pipe Insulation, a dense but soft foam used for insulating pipes (see below for a link.) First, the wound should not be wet before wrapping. After applying a Hydrogel dressing, I cover with a primary dressing being 4-inch Gauze bandage product called Elastikon wrap which is ideal for hard to bandage areas. Once the wound is protected, then I place the appropriately sized diameter Tube Pipe Insulation (it already is split to wrap around a pipe) around the wounded section on the tail and bind it to the tail (which is fully covered with hair) with Duct Tape which is taped over an area covered with Vet Wrap. See below for link to Vet Wrap. This is to prevent the Duct tape from tearing out all the dogs hair on the tail each time you remove the pipe insulation to change the bandages (daily.) The Duct Tape is wrapped onto Vet Wrap which covers the hair and bony tail both above and below the wound. The downside is that the foam pipe fitting, though soft and protective, does not permit air circulation which I worry about and so one must be diligent and vigilant about changing the bandages and, yes, constantly smelling the wound to make certain it is not becoming infected.
But, how do you prevent the dog from wagging the tail so that the pipe fitting does not sail across the room? Well, I came across an interesting medical device that may present itself as a possible solution for tail injuries. The product is not designed for a tail but looking at it more closely I believe it might work. It is called a Rear Leg Hobble System manufactured by DogLegges. I use this company for medical boots on foot wounds (see my Blog Post "Dog Foot Pad Injuries" and, if necessary, elbow hygromas (see my Health Page Other Common Disorders or Ailments.) The rear leg hobble system appears as if the one end of the hobbler could be connected to the tail above the wounded region and the other end hobbled above the hock as the hobble strap length is adjustable. The product illustrates the use for hobbling a Poodle with a short tail, however, this product is custom made to the specific size of the dog. Wolfhounds have long tails, so, it may work but you would need to speak directly with the company. Notably though, if you use the hobble system as a tool to connect the tail to the upper leg then most likely you do not have to use the tube pipe insulation over the bandaged wound. If you have questions feel free to reach out to me.
One other idea set forth by a member of the Irish Wolfhound Club of America is included on the IWCA website with a link called Tail Sling. It is a simplistic approach so check it out but I do worry about a lack of air circulation around the wound as it depicts the wound completely covered in the sweatpants.
If you haven't done so, please read the Vetruus website on the split tail as it provides interesting insight on a dog who recovered beautifully after using the Dog Ends devices.
Facts About Caloric Density and Carbohydrates vs Protein Levels in Giant Breed Puppy Food
The topic of protein levels in giant breed puppy food is one that I have meant to discuss. First off, it is a myth that high protein levels cause damage to the long bones of a growing, giant breed puppy. Most people who feed commercially prepared dry dog food are misguided by this urban tale.....
Recently, I received a call from a new Wolfhound puppy owner who was seeking advice. During the conversation, the gentleman expressed his concern about protein levels in dog food. He informed me that he purchased a premium bag of dog food with a low protein level of 22%, as he was told that high levels of protein are not recommended for giant breed puppies as it can cause damage to their growing bones.
The topic of protein levels in giant breed puppy food is one that I have meant to discuss. First off, it is a myth that high protein levels cause damage to the long bones of a growing, giant breed puppy. Most people who feed commercially prepared dry dog food are misguided by this urban tale.
Instead, what should be one of the most pressing and harmful issues occupying people's minds about commercially prepared dog food designed for giant breed puppies is not protein BUT caloric density and the sources from which these calories are derived. As well as the high-density percentages of carbohydrates. In contrast, those who are entirely unperturbed about protein levels are those people who "Naturally Rear," as I do, where the protein sources are fresh, raw meat or poultry, fish, along with oats, yogurt, vegetables and so on.
Due to space limitations, I can only provide a review on this mainstream misconception as it could fill pages and pages. So, here goes.
Rapid growth stresses developing bones and joints. What can cause rapid growth is feeding a calorically dense and high carbohydrate diet which will make a pup grow too quickly; faster than their developing long bones and articulating joints can accommodate and will result in skeletal abnormalities.
Typically, as a pup evolves the bones and muscles should mature together in harmony, but bones that grow much too fast will be less dense and weaker than ones growing at a more appropriate rate. Weaker bones, in turn, creates issues for giant breeds who carry more weight in which such pup(s) will experience the causal factors of artificial nutrition.
What about protein? Protein is a source of energy. A point of fact is that growing puppies require more protein than an adult dog which contradicts the urban tale. Proteins are essential for building blocks of all tissues and organs, to include tendons, ligaments, cartilage, and muscle contraction. Yes, too much protein can be detrimental to healthy growth due to an imbalance of calcium and phosphorus which affects the long bones and joints. However, this is not always the culprit in commercially prepared puppy food. Why? Read on as down below I reveal some compelling relatively unknown information about the actual amounts of protein in such foods and their sources. What are the primary culprits in puppy as well adult dog food?
Most commercial dry dog foods contain at least 50% carbohydrates and sometimes more than 15% crude fiber. Let me quickly address crude fiber as this amount is at least three times the recommended amount according to the Mark Morris Institute who publishes the Small Animal Clinical Nutrition, 5th Edition on commercial pet foods. This book further reports that in excess, crude fiber reduces the energy and nutrients in the food whereas the dog has difficulty eating enough food to satisfy his nutritional needs. In other words, dogs consuming much of today's inferior, low digestibility commercial foods will devour large quantities of food, but the high amount of fiber within the diet can decrease mineral absorption. Thus, it does not matter how much the dog eats; he cannot absorb the necessary minerals because there is too much fiber.
Carbohydrates. Many commercial brand dog foods have high caloric density derived not just from fat but carbs. The principal function of carbohydrates is to provide structural integrity as they work as a binder holding the ground meal in shape. I already stated that most all dog foods are at least 50% carbohydrates, and it would be unusual for a dry pet food to be formulated with fewer than 40% carbohydrates because of the minimum requirement for extrusion or shaping through a die, as told by the Small Animal Clinical Nutrition, 5th Edition.
Incidentally, canines do not have the same enzymes as humans so they can only process carbohydrates very, very slowly. Importantly, the abundance of carbohydrates (sugars and starches) contained in commercial dog foods is a significant factor in canine dental disease and tartar build-up. Moreover, dental disease and heart disease can go hand in hand.
Here are some examples of carbohydrate concentrations commonly found in commercial dog food:
Rice Flour 90%
Rice 90%
Corn Flour 85%
Corn Starch 88%
Corn 81%
Grain Sorghum 80%
Wheat Flour 82%
Wheat 78%
Calories and fat. Both of these can present a bit of a dilemma for some companies. Typically, to dilute the number of calories in commercially prepared dog food, the manufacturer adds increased fiber, insoluble fiber such as cellulose and peanut hulls, to the processing. However, because crude fiber behaves as an anticaking agent, it simultaneously causes high friction during the extrusion or shaping process. So, the manufacturer has to add fat back into the ingredients so the mixture, commonly known as slurry, can be processed more efficiently. While adding fat back in sometimes can neutralize or minimize the fiber's primary purpose of reducing calories. According to Small Animal Clinical Nutrition, 5th Edition; "Fats contribute calories at 2.25 times the rate of carbohydrates or proteins, and the use of fat ingredients is the most efficient method of increasing the energy density of food to limit a pet’s consumption of other nutrients."
Back to the question of protein. There is an even lesser known truth about the actual amount of meat as listed on the dog food's label.
Again citing the Small Animal Nutrition 5th Edition, the United States has labeling regulations that stipulate ingredients must be listed in order of weight predominance. Of course, wet meat weighs more than dry meat, so, manufacturers use the wet weight of the meat or poultry that elevates or places the protein within the label's top three ingredients. They do so by incorporating fresh or frozen meat/poultry into the dry extruded dog food using a slurry composed of animal tissues, fat, and water, which is grounded and mixed in a separate tank. The water in the meat (60 to 70%), however, must first be dried off to make a dry product. Consequently, the actual amount of meat or poultry ingredients would be listed much farther down on the label if it were added as a dry meat meal.
Be aware that manufacturer claims that the "meat based" dog food has a high-meat content is not always accurate. Also, dog food ingredient labels list other sources that protein may also be derived from such as dried egg, rice gluten, corn gluten, and soybean meal.
The long and short of it is that densely packed carbohydrates in complete dog food along with high fats increase the caloric density, and this should be the worrisome factor that can cause health problems in growing giant breed puppies. All of this is not to say that an owner who feeds only meat and bone without other essential ingredients that provide nitrogen, minerals, calcium, phosphorus, and so on is doing the right thing. I utilize oats in my hound's diets along with all the other key components of "Natural Rearing" for a balance of nutrition. Nonetheless, I can assure you that my giant breed pups consume much higher amounts of protein than any bag of manufactured puppy food, but they do so in the fresh, raw variety. Never a slurry of animal tissues, fat, and water.